21 November 2022: Clinical Research
Long-Term Effect of Pancreaticoduodenectomy Combined with Revascularization for Resectable Pancreatic Carcinoma in Elderly Patients
Jiali Yang1ABCDEF, Zhengrong Xu2ABCD, Junfeng Zhang1CD, Yao Zheng1CD, Jianyou Gu1AC, Qiang Zhou1CD, Xianxing Wang1CD, Shixiang Guo1DF, Hongyu Zhang3AD, Shengkai Chen1ADG*, Huaizhi Wang1ADGDOI: 10.12659/MSM.938443
Med Sci Monit 2022; 28:e938443
Abstract
BACKGROUND: Pancreaticoduodenectomy combined with revascularization (PDR) is the main surgical procedure for resectable pancreatic ductal adenocarcinoma (PDAC) with venous system invasion, but this procedure is discouraged in elderly patients because of physical complexity. Our aim was to explore the differences of perioperative and survival in patients of different ages who underwent PDR.
MATERIAL AND METHODS: We reviewed data from PDAC patients undergoing PDR from 2007 to 2018. Patients were subdivided into 3 groups according to age: <60 years, 60-70 years, and ≥70 years. Postoperative complications and long-term survival were compared among the 3 groups.
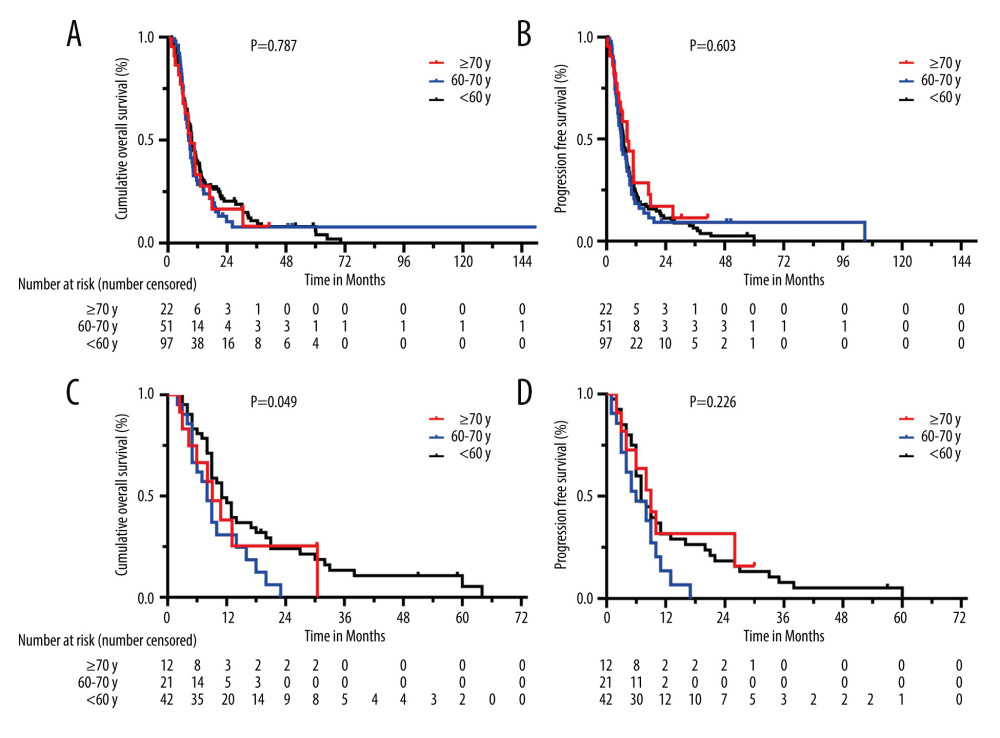
RESULTS: From 626 patients, 185 had en bloc venous resection who underwent PDR (103, 55, and 27 patients from young to elderly). Increasing age was linked to a higher prevalence of ICU management (P=0.035) and more serious complications (grade ≥III, P=0.043); overall mortality was 8.1% and did not significantly differ among age-matched groups. Further, there was no difference in overall survival (OS) or progression-free survival (PFS) based on age (<60, 60-70, ≥70, median OS were 9.7, 8.4 vs 9.1 months, respectively, P=0.787; median PFS were 6.9, 6.1 vs 8.4 months, respectively, P=0.603). However, patients <60 years whose tumors invaded the superior mesenteric vascular had better survival outcomes when compared with the other 2 groups (11.5 vs 8.4, 9.1 months, P=0.049).
CONCLUSIONS: The results show that age should not be considered an absolute contraindication for PDR, as elderly patients can achieve the same surgical efficacy and long-term survival prognosis.
Keywords: Survival Prognosis, complications, the elderly, revascularization, pancreatic adenocarcinoma, Humans, Aged, Middle Aged, Pancreaticoduodenectomy, Portal Vein, Pancreatectomy, Pancreatic Neoplasms
Background
Pancreatic ductal adenocarcinoma (PDAC) is a deadly disease that is predicted to become the second leading cause of cancer-related death in the United States by 2030, and the 5-year survival rate remains low, at 0–10.8% [1]. The Surveillance, Epidemiology, and End Results (SEER) Cancer Statistics Review states that pancreatic carcinoma is predominantly a disease of the older population, rarely occurring before the age of 40 years [2]. Indeed, the risk of developing pancreatic cancer has been shown to increase with age, with the highest peak occurring between 60 and 80 years of age [3]. In China, both the incidence (ASR: 5.02/105 in 2017) and mortality (ASR: 5.67/105 in 2017) of pancreatic cancer were the highest in the population aged 85–90 years [4]. Therefore, age should not be ignored in the diagnosis and treatment of pancreatic cancer.
Major pancreatic surgery for PDAC is justified in elderly patients [5]. Previous studies have shown that a higher rate of preoperative comorbidities in elderly patients (>75 years) tended to increase the rate of nonsurgical postoperative complications (
Nevertheless, there are few reports on the influence of age over 60 years on the safety and survival benefits of PDAC after PDR. This highlights the need for both multidisciplinary treatments for patients of an advanced age as well as suitable approaches for stratifying patients according to the most effective treatment regimen. Due to the perceived frailty of elderly individuals, we retrospectively compared the outcomes of the late elderly (≥70), young elderly (60–70) and younger (<60) patients who had undergone PDR for PDAC at our medical center during the past 12 years to determine whether it is safe, feasible, and worthwhile for the elderly patient population.
Material and Methods
STUDY DESIGN:
This was a retrospective review of all consecutive patients with PDAC who had undergone curative PDR at our medical center between January 1, 2007, and October 31, 2018. Preoperative, intraoperative, and postoperative data are continuously documented for intra- and extra-clinical benchmarking. The series of patients was divided into 3 groups according age: group A, <60 years; group B, 60–70 years; and group C, ≥70 years. None of the patients had received radiotherapy or chemotherapy before surgery. The inclusion criteria were assessed for resectable pancreatic head adenocarcinoma by the surgery and radiological specialist according to the National Comprehensive Cancer Network (NCCN) definitions and no other concomitant cancer. Patients with pancreatic body/tail tumors, periampullary carcinoma, cholangiocarcinoma, duodenal adenocarcinoma, neuroendocrine tumors, or other histology were excluded. This study was approved and supervised by the Ethics Committee of Southwest Hospital, Third Military Medical University, Chongqing, China.
DATA ACQUISITION:
All patients who underwent contrast-enhanced CT and/or MRI were performed on an individual basis preoperatively, and then en bloc resection of PDR with associated lymphadenectomies was performed by experienced pancreatic surgeons. Clinical data were extracted from the medical records, including preoperative examination data (epidemiological information and laboratory values, as shown in Table 1) [9], intraoperative features (location of vascular invasion, modes of reconstruction, duration of operation, and blood loss, as shown in Table 2), and postoperative complications (pancreatic fistula [10], biliary fistula, delayed gastric emptying [11] and others [12]). Furthermore, we focused on the resection margin status, lymph node status, presence of perineural invasion and vascular infiltration, extent of distant metastasis, and degree of differentiation in the histopathologic analysis, and then these patients were staged according to the 8th edition of the American Joint Committee on Cancer [13].
The preoperative CT/MRI imaging examinations and the features observed during intraoperative exploration were the determining factors for the selection of segmental vascular resection. Reconstruction of PV, SMV, or confluence of PV-SMV included primary closure, end-to-end anastomosis, and an interposition graft dictated by anatomical necessity. Vital status was collected based on the last follow-up visit or telephone consultation, and the follow-up period ended in May 2021.
STATISTICAL ANALYSIS:
Statistical analysis was performed using univariate analysis in combination with multivariate analysis. Categorical variables are presented as percentages and were compared using the chi-squared test. Continuous variables are presented as medians (ranges) and were analyzed using the one-way ANOVA or Kruskal-Wallis test according to normally distributed or non-normally distributed data. OS of those who had PDR was estimated by Kaplan-Meier survival curves and compared using the log-rank test. Multivariable analyses used Cox proportional hazards regression models. All statistical tests were two-tailed, and
Results
POPULATION CHARACTERISTICS:
Over the past 12 years, a total of 626 patients with pancreatic head adenocarcinomas have undergone open pancreaticoduodenectomy at our center, and 185 patients (29.6%) who underwent en bloc PDR and best supportive care were included in this study. The median age was 58 years (interquartile range, IQR 33–80): 103 patients (55.7%, median 50, IQR 33–59) were <60 years, 55 patients (30%, median 63, IQR 60–69) were between 60 and 70 years, and 27 patients (14.6%, median 71, IQR 70–80) were aged ≥70 years. Table 1 outlines the demographic and clinical presentations of the 3 groups. Among them, there were statistically significant differences in NRS 2002 score, ASA classification, and concomitant comorbidity, which is reflected in a higher NRS 2002 score and ASA stage and the presence of previous hypertension, coronary artery disease, and COPD in the elderly patients (group C). However, tobacco and alcohol use, history of abdominal surgery, preoperative jaundice and biliary drainage, and preoperative laboratory values were not significantly different among the 3 groups.
PERIOPERATIVE HOSPITALIZATION AND PATHOLOGIC DIAGNOSIS:
The type of PD includes the classic Whipple procedure or PPPD combined with vein resection and reconstruction. The surgical outcomes of the different age groups are shown in Table 2. The intraoperative values of multiple parameters, such as vascular invasion site, types of venous reconstruction, ligation of splenic vein, combined organ resection, operation duration, blood loss, transfusion and postoperative hospital stay, did not increase with age. Additionally, comparing group A with group B (41.7% and 40%, respectively), tumor invasion into the SMV was more commonly observed in elderly patients (group C: aged ≥70 years, 51.9%). Regardless of the site of vascular invasion, the most common form of vascular reconstruction used during surgery was end-to-end anastomosis, which was performed in 51 patients (49.5%) who were <60 years (group A), 30 patients (54.5%) who were between 60 and 70 years (group B), and 70 patients (74.1%) who were ≥70 years (group C). However, elderly patients were more likely to require intensive care unit (ICU) management (P=0.035, Table 2).
All the enrolled patients in this study had a proven histological diagnosis of pancreatic head ductal adenocarcinoma. Statistical analysis of 185 patients revealed that there was no difference among the 3 age groups in terms of tumor size, differentiation, pathological invasion of PV-SMV, neurological invasion, resection margin, or TNM staging (Table 2).
POSTOPERATIVE COMPLICATIONS:
A total of 114 patients (61.6%) experienced postoperative complications of different grades, of whom 15 patients (8.1%) died within 90 days; namely, 6 patients (5.8%) in group A, 4 patients (7.3%) in group B and 5 patients (18.5%) in group C, with no significant difference observed among the groups. With regard to surgery-related death, the top 2 most common causes were intra-abdominal hemorrhage (9, 60%) and pulmonary infection (5, 35.7%).
Surgery-related overall complications were similar across all 3 age groups according to the Clavien-Dindo classification (61.2%, 61.8%, and 63%, respectively), but more serious complications (grade ≥III) occurred mainly in the late elderly group (≥70 years, 33.3%) than in the other groups (12.6% and 12.7%, P=0.043), and these results may be related to the incidence of postoperative organ dysfunction and pulmonary infection in the late elderly group. However, the rates of relevant postoperative grade V complications were similar in different age groups. Further subdivision of the patients based on the type of complication (pancreatic fistula, non-pancreatic anastomotic leakage, lymphatic leakage, DGE, hemorrhage, blood transfusion for non-hemorrhagic anaemia, thoracic or abdominal puncture and drainage, thoracic or abdominal puncture and drainage, intraperitoneal infection, and re-laparotomy) revealed that there were no significant differences across the different age groups. In addition, we noted a statistically significant difference in the rate of pulmonary infection (P=0.002) but not the rate of overall infections (P=0.239), which may be because 4 patients had both pulmonary infection and intraperitoneal infection. Interestingly, the patients aged ≥70 years had a lower incidence of non-pancreatic anastomotic leakage, DEG grade B/C, and post-pancreatectomy hemorrhage grade A/B (Table 3).
SURVIVAL ANALYSIS:
At follow-up, a total of 170 patients (91.9%) in the study group who underwent PDR for PDAC achieved the expected postoperative recovery. By the follow-up date of May 2021, 151 patients had died due to cancer-specific causes, 156 had developed tumor recurrence, and 19 patients (11.2%) were censored for nearly 14 years (14 patients survived, and 5 patients were lost to follow-up). The overall median follow-up time was 51.9 months (IQR: 30.4–157.1, 95% Cl: 46.786–57.014). The median OS time was 9.2 months (IQR: 5.9–17.9, 95% Cl: 8.169–10.231), and the 0.5-, 1-, 2-, 3-, 4-, and 5-year OS rates were 74.1%, 35.3%, 17.1%, 9.8%, 8.0%, and 6.6%, respectively. The median PFS time was 6.7 months (IQR: 3.8–11.2, 95% CI: 5.573–7.827), and the 0.5-, 1-, 2-, 3-, 4-, and 5-year PFS rates were 55.8%, 22.0%, 11.02%, 7.1%, 4.1%, and 2.4%, respectively. We further plotted the K-M curves of the OS and PFS of patients at different age stages, and the results showed that age was not related to these factors (Figure 1). The median OS was 9.7 months, 8.4 months, and 9.1 months for patients aged <60 years, 60 years ≤ age <70 years to ≥70 years, respectively, with a P value of 0.787. The median PFS was 6.9 months, 6.1 months, and 8.4 months, with a P value of 0.603 (Figure 1A, 1B).
In contrast, significantly longer OS was associated with postoperative adjuvant antineoplastic therapy (12.9 vs 7.9 mo. HR=0.470, 95% CI: 0.329–0.670, P=0.000) in all age groups. To assess the influence of these prognostic factors, we assessed OS and PFS for patients in the different age groups (Table 4). In our series, compared to older patients preoperatively diagnosed with PDAC and SMV invasion, younger patients had better OS outcomes (11.5 vs 8.4 and 9.1 months, Figure 1C), but there was no difference in PFS among the 3 patient groups (7.2 vs 6.2 and 8.4 months, Figure 1D). Other independent risk factors affecting long-term outcomes were not related to age.
Discussion
In this retrospective analysis, data on 185 PDAC patients who underwent PDR from our center were analyzed. The patients were divided into 3 groups according to age: the late elderly group (≥70), the young elderly group (60–70), and the younger group (<60). Then, we explored the difference and prognosis after PDR in different age groups. The analysis suggested that late elderly patients had a higher NRS 2002, more comorbidities, and an increased risk of anesthesia than their younger counterparts. However, these preferences did not affect the incidence of postoperative complications and mortality in patients of different ages, nor did they affect OS and PFS.
The incidence and overall mortality of PDAC correlate with increasing age and are slightly higher in men than in women [14]. It is occasionally difficult to make treatment decisions for elderly patients because physicians base their treatment decisions on physical function, the comorbidity of the patient, the progression of the tumor, and their personal willingness to receive treatment. Growing evidence has demonstrated that PDR is as safe and effective as PD for patients with PDAC [15,16]. Median survival was found to be significantly longer among patients undergoing PD or PDR than in those undergoing palliative operation (surgical bypass,
Predictably, patients aged 70 and older had a higher NRS 2002 score, higher anesthesia risk, and more preoperative complications than other age groups. But, considering overall postoperative complications, our data do not confirm the previously reported findings of an overall higher incidence of complications in the elderly population [18,19]. However, there was a significant difference in the incidence of grade III or higher complications according to age. Compared with patients in the 2 relatively young groups, the late elderly group was more likely to experience advanced complications (n=9, 33.3%), organ dysfunction (n=8, 29.6%), and pulmonary infection (n=10, 37%). This may be associated with organ degeneration and the level of vulnerability of the elderly. A study of immunonutritional and physical indices in elderly individuals suggested that individuals >80 years old who underwent PD had a significantly higher neutrophil-lymphocyte ratio and a lower prognostic nutritional index, reduced muscle strength, and impaired walking ability [20]. Pancreatic leakage is the most concerning complication after pancreatic surgery [21]. Our study did not conclude that elderly patients with PDAC had a higher risk of pancreatic fistula, which is consistent with results from other large-cohort studies [22,23].
Previous scholars have observed that elderly patients with surgically resected pancreatic carcinoma have a significant decrease in overall survival with increasing age [24,25]. Li and Liu’s study reported that the age limit was 60 years [2]. In our retrospective study, the median OS and PFS were not significantly different at 60 and 70 years old, respectively, and age was not found to be a contraindication for PDR. In addition to assessing the effect of TNM staging, the degree of differentiation, and postoperative adjuvant antineoplastic therapy, we further explored whether different vascular invasion sites on the PV-SMV axis have a different influence on prognosis and survival. Patients aged <60 years who had invasion into the SMV trunk had a longer survival time (11.5 mo.) than with the 60–70 age group and ≥70 age group (8.4 months and 9.1 months), and
To prolong long-term survival, adjuvant therapy is indispensable. Considerable controversy remains over whether patients should undergo preoperative neoadjuvant therapy for borderline resectable PDAC [27]. This retrospective study was also conducted in accordance with the principle of early surgery, and the results showed that adjuvant therapy after PDR had no effect on long-term survival, regardless of age. Nevertheless, as age increased, the number of patients receiving adjuvant therapy gradually decreased: 43 (44.3%), 17 (33.3%), and 5 (22.7%), respectively. Elderly patients are often discouraged from receiving adjuvant therapy because of adverse events, and most of them fail to finish the whole chemotherapy regimen. In fact, other researchers have shown that elderly patients suffer a higher incidence of severe adverse events (50% vs 28.3%,
Several limitations of our study should be acknowledged. First, there is inevitably a patient selection bias because our center treats patients who are seriously ill, as well as those who are transferred from other hospitals due to comorbidities and their overall level of fitness. Second, this was a single-center review with a small sample size, which in turn may limit the applicability of our results to other populations. Third, we did not assess the role of neoadjuvant therapy. Future studies, preferably larger patient cohorts from multiple centers, are needed to further confirm our preliminary conclusions.
Conclusions
In summary, the current study demonstrated that advanced age is not an independent contraindication to PDR. Regardless of the age of the patient undergoing PDR, there was no difference in postoperative complications or long-term survival benefits (OS and PFS), but the severity of complications (grade ≥III) was higher for patients older than 70 years than for younger patients. Importantly, it is necessary for late elderly patients with PDAC to be evaluated by a multidisciplinary team of physicians before undergoing PDR.
Tables
Table 1. Comparison the demographic and clinical characteristics of the PDAC patients who underwent PDR according to age.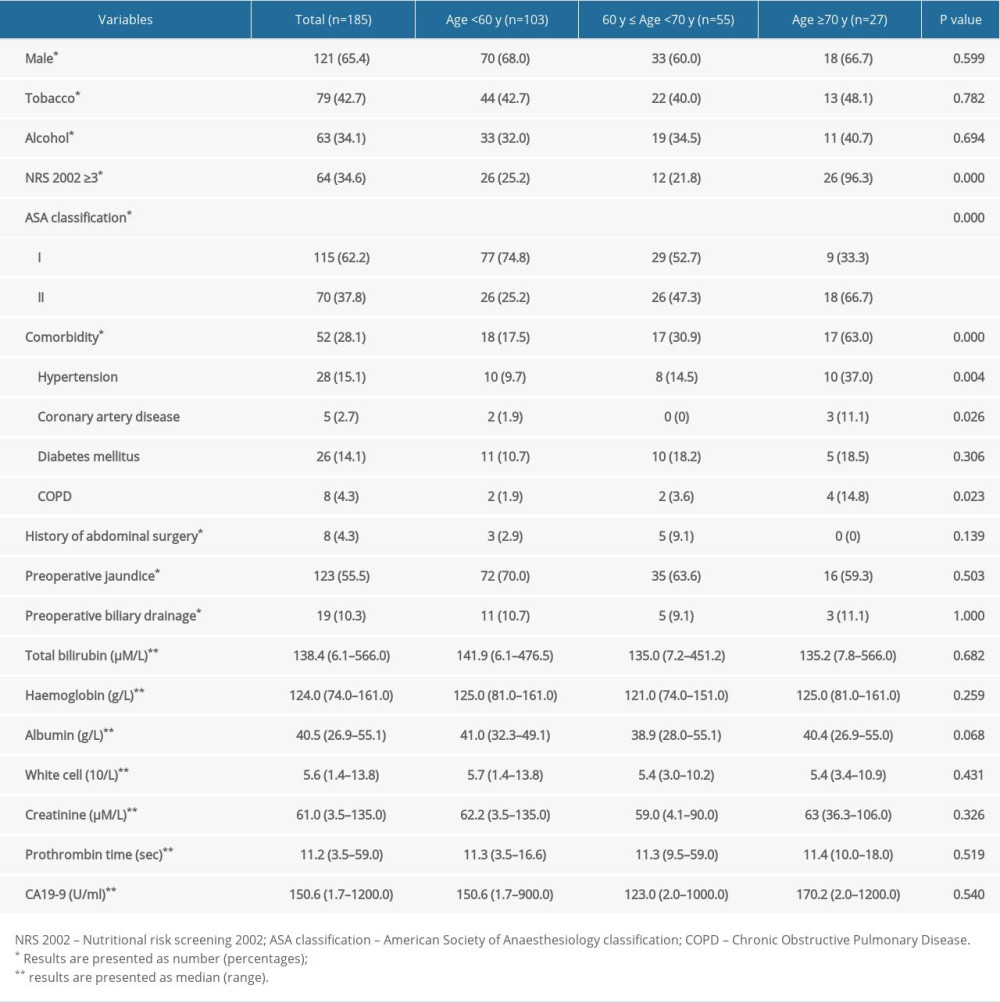 Table 2. Perioperative and pathologic characteristics of the PDAC patients who underwent PDR according to age.
Table 2. Perioperative and pathologic characteristics of the PDAC patients who underwent PDR according to age.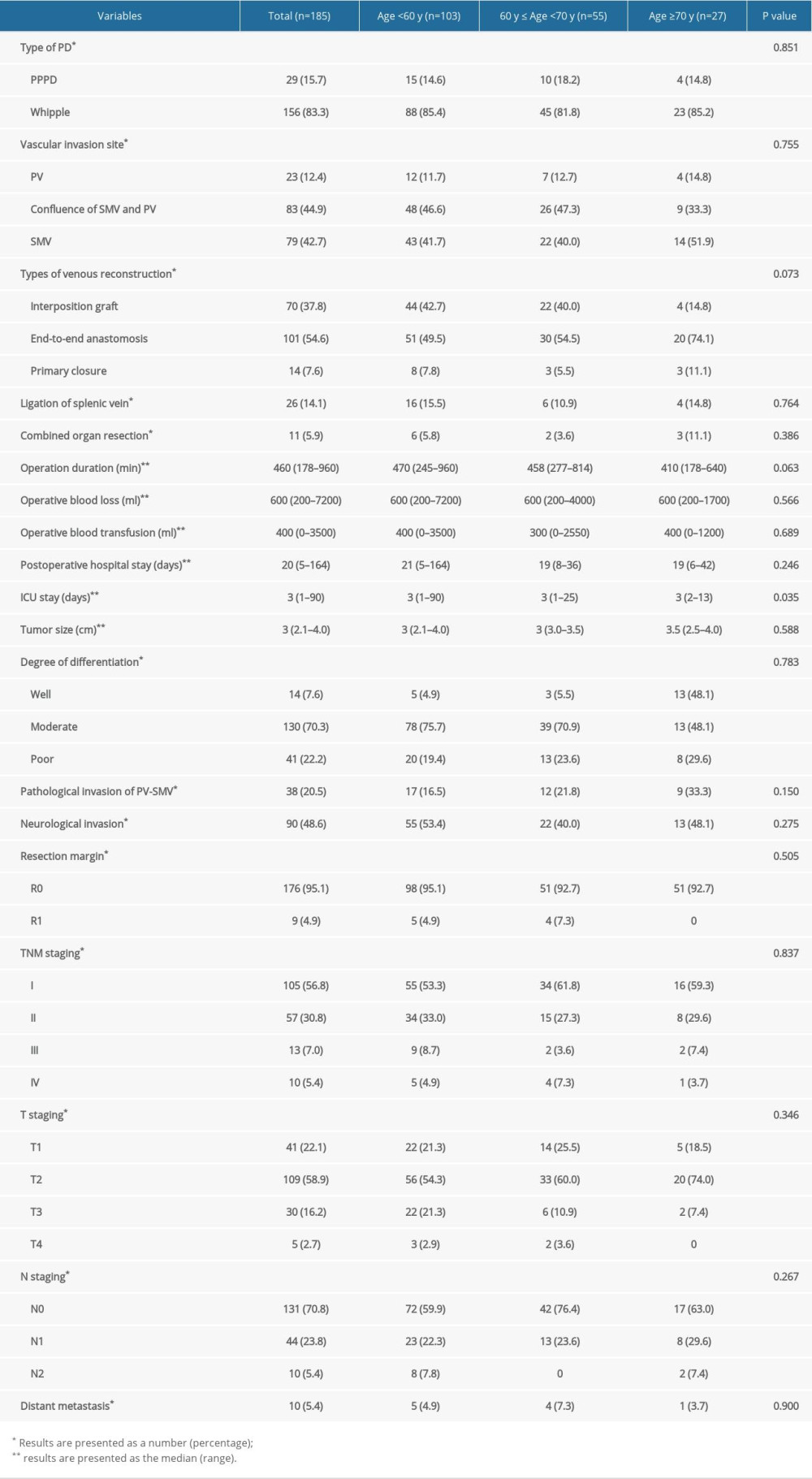 Table 3. Postoperative complications of stays the PDAC patients who underwent PDR according to age.
Table 3. Postoperative complications of stays the PDAC patients who underwent PDR according to age.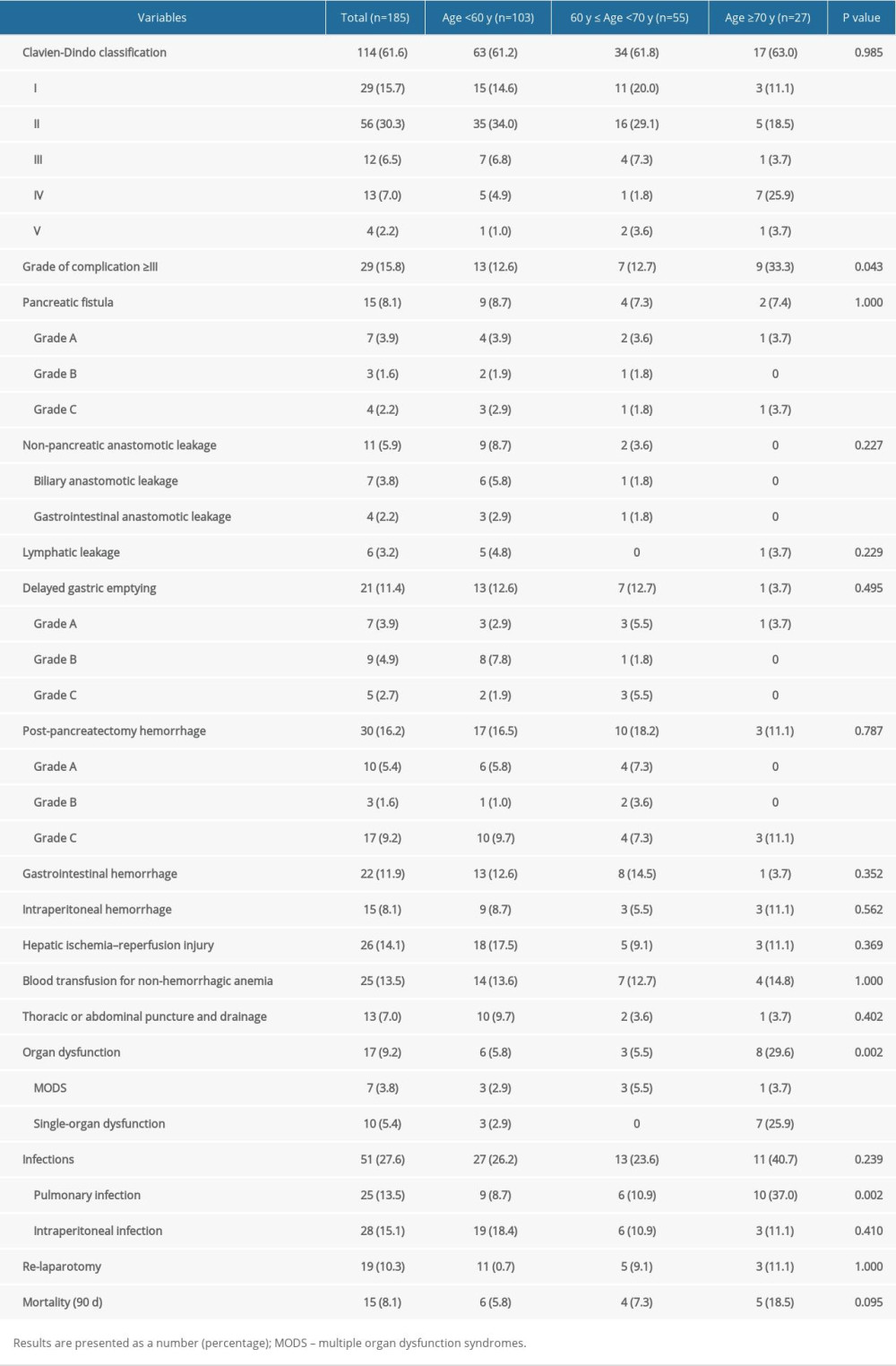 Table 4. Analysis of the OS and PFS of PDAC patients who underwent PDR according to age.
Table 4. Analysis of the OS and PFS of PDAC patients who underwent PDR according to age.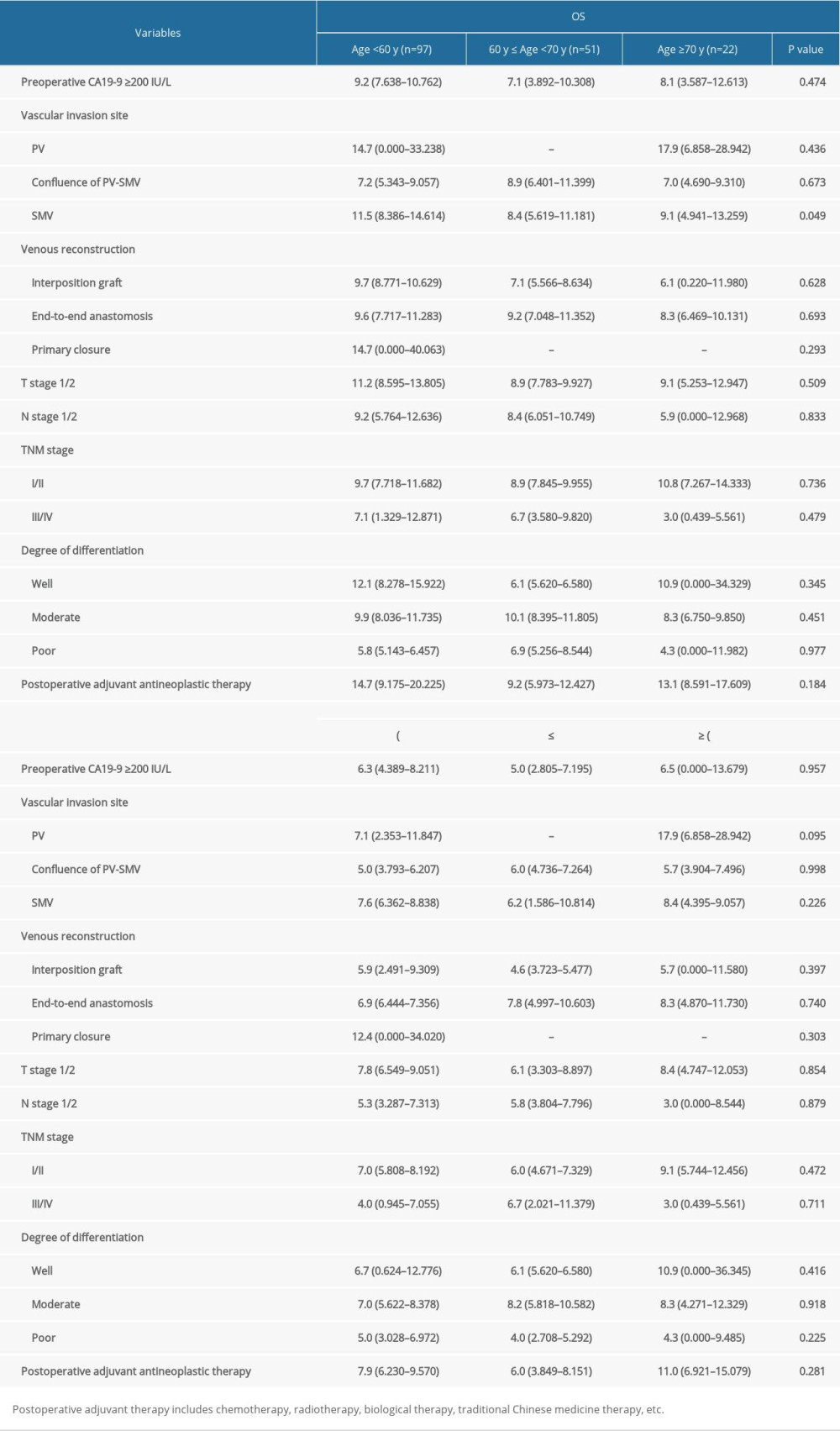
References
1. Wood LD, Canto MI, Jaffee EM, Simeone DM, Pancreatic cancer: Pathogenesis, screening, diagnosis, and treatment: Gastroenterology, 2022; 163; 386-402e1
2. Li J, Liu L, Overall survival in patients over 40 years old with surgically resected pancreatic carcinoma: A SEER-based nomogram analysis: BMC Cancer, 2019; 19; 726
3. Rawla P, Sunkara T, Gaduputi V, Epidemiology of pancreatic cancer: Global trends, etiology and risk factors: World J Oncol, 2019; 10; 10-27
4. Cai J, Chen H, Lu M, Advances in the epidemiology of pancreatic cancer: Trends, risk factors, screening, and prognosis: Cancer Lett, 2021; 520; 1-11
5. Kim SY, Fink MA, Perini M, Age 80 years and over is not associated with increased morbidity and mortality following pancreaticoduodenectomy: ANZ J Surg, 2018; 88; E445-50
6. Renz BW, Khalil PN, Mikhailov M, Pancreaticoduodenectomy for adenocarcinoma of the pancreatic head is justified in elderly patients: A Retrospective Cohort Study: Int J Surg (London, England), 2016; 28; 118-25
7. Murakami Y, Satoi S, Motoi F, Portal or superior mesenteric vein resection in pancreatoduodenectomy for pancreatic head carcinoma: Br J Surg, 2015; 102; 837-46
8. Traub B, Link KH, Kornmann M, Curing pancreatic cancer: Semin Cancer Biol, 2021; 76; 232-46
9. Kondrup J, Rasmussen HH, Hamberg O, Stanga Z, Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials: Clin Nutr, 2003; 22; 321-36
10. Bassi C, Marchegiani G, Dervenis C, The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after: Surgery, 2017; 161; 584-91
11. Healy JM, Kunstman JW, Salem RR, Proposal and critical appraisal of exclusion criteria to the international study group for pancreatic surgery definition of delayed gastric emptying: J Am Coll Surg, 2015; 220; 1036-43e1
12. Wente MN, Veit JA, Bassi C, An International Study Group of Pancreatic Surgery (ISGPS) definition: Surgery, 2007; 142; 20-25
13. Chun YS, Pawlik TM, Vauthey JN: Ann Surg Oncol, 2018; 25; 845-47
14. Zheng R, Zhang S, Zeng H, Cancer incidence and mortality in China, 2016: Journal of the National Cancer Center, 2022; 2; 1-9
15. Barreto SG, Windsor JA, Justifying vein resection with pancreatoduodenectomy: Lancet Oncol, 2016; 17; e118-e24
16. Xie ZB, Li J, Gu JC, Pancreatoduodenectomy with portal vein resection favors the survival time of patients with pancreatic ductal adenocarcinoma: A propensity score matching analysis: Oncol Lett, 2019; 18; 4563-72
17. Ravikumar R, Sabin C, Abu Hilal M, Portal vein resection in borderline resectable pancreatic cancer: A United Kingdom multicenter study: J Am Coll Surg, 2014; 218; 401-11
18. Kleive D, Sahakyan MA, Berstad AE, Trends in indications, complications and outcomes for venous resection during pancreatoduodenectomy: Br J Surg, 2017; 104; 1558-67
19. Sun JW, Zhang PP, Ren H, Hao JH, Pancreaticoduodenectomy and pancreaticoduodenectomy combined with superior mesenteric-portal vein resection for elderly cancer patients: Hepatobiliary Pancreat Dis Int, 2014; 13; 428-34
20. Sugimachi K, Iguchi T, Mano Y, The impact of immunonutritional and physical status on surgical outcome after pancreaticoduodenectomy in elderly patients: Anticancer Res, 2019; 39; 6347-53
21. Liu FH, Jiang XZ, Huang B, Yu Y, Preoperative computed tomography imaging of the pancreas identifying predictive factors for the progression of grade a, or biochemical leak, to grade B postoperative pancreatic fistula following pancreaticoduodenectomy: a retrospective study: Med Sci Monit, 2021; 27; e928489
22. Pędziwiatr M, Małczak P, Mizera M, Pancreatoduodenectomy for pancreatic head tumors in the elderly – systematic review and meta-analysis: Surg Oncol, 2018; 27; 346-64
23. van der Heijde N, Balduzzi A, Alseidi A, The role of older age and obesity in minimally invasive and open pancreatic surgery: A systematic review and meta-analysis: Pancreatology, 2020; 20; 1234-42
24. Wiltberger G, Muhl B, Benzing C, Pancreaticoduodenectomy in the elderly patient: Age-adapted risk assessment: Dig Surg, 2017; 34; 43-51
25. Paiella S, De Pastena M, Pollini T, Pancreaticoduodenectomy in patients ≥75 years of age: Are there any differences with other age ranges in oncological and surgical outcomes? Results from a tertiary referral center: World J Gastroenterol, 2017; 23; 3077-83
26. Ravikumar R, Sabin C, Abu Hilal M, Impact of portal vein infiltration and type of venous reconstruction in surgery for borderline resectable pancreatic cancer: Br J Surg, 2017; 104; 1539-48
27. Katz MHG, Varadhachary GR, Borderline resectable pancreatic cancer – at the crossroads of precision medicine: Cancer, 2019; 125; 1584-87
28. Li X, Huang DB, Zhang Q, The efficacy and toxicity of chemotherapy in the elderly with advanced pancreatic cancer: Pancreatology, 2020; 20; 95-100
29. Watanabe Y, Shinkawa T, Endo S, Long-term outcomes after pancreatectomy for pancreatic ductal adenocarcinoma in elderly patients: Special reference to postoperative adjuvant chemotherapy: World J Surg, 2018; 42; 2617-26
30. Kamarajah SK, Sonnenday CJ, Cho CS, Association of adjuvant radiotherapy with survival after margin-negative resection of pancreatic ductal adenocarcinoma: A propensity-matched National Cancer Database (NCDB) analysis: Ann Surg, 2021; 273; 587-94
31. van Roessel S, van Veldhuisen E, Klompmaker S, Evaluation of adjuvant chemotherapy in patients with resected pancreatic cancer after neoadjuvant FOLFIRINOX treatment: JAMA Oncol, 2020; 6; 1733-40
Tables
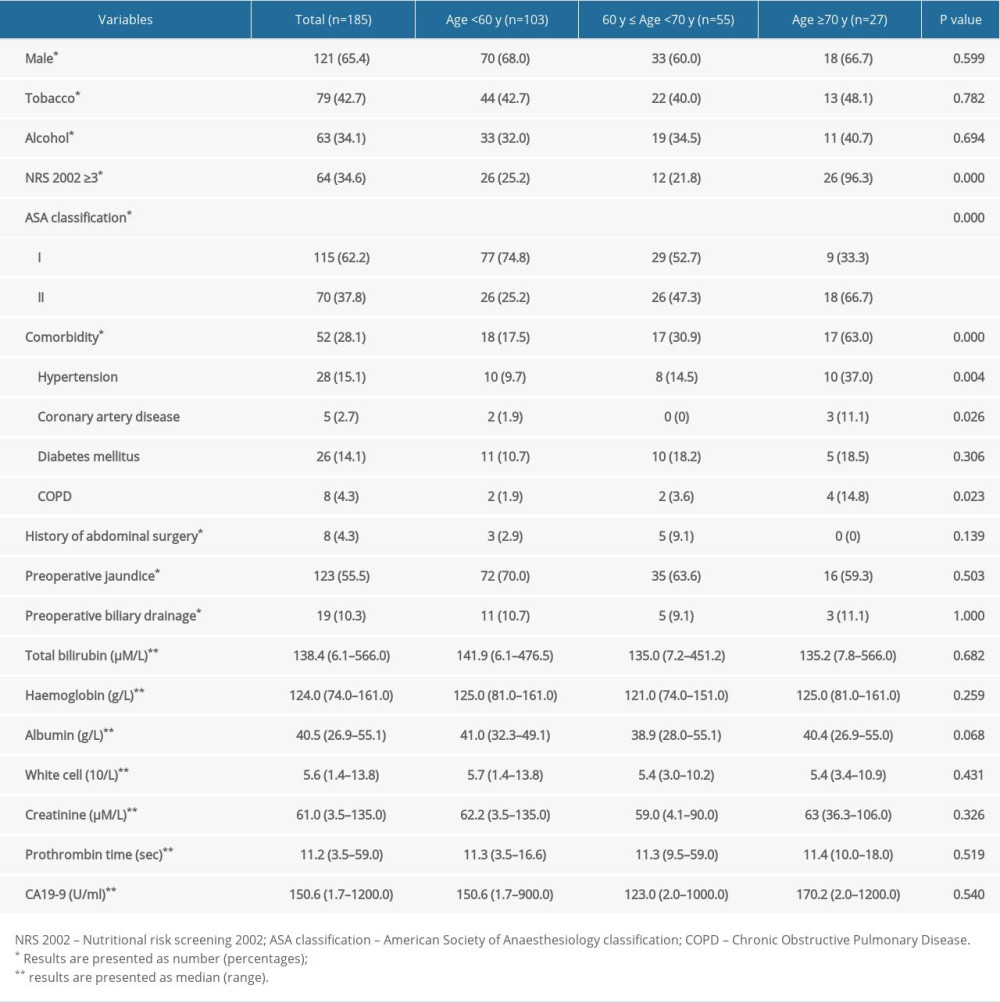 Table 1. Comparison the demographic and clinical characteristics of the PDAC patients who underwent PDR according to age.
Table 1. Comparison the demographic and clinical characteristics of the PDAC patients who underwent PDR according to age.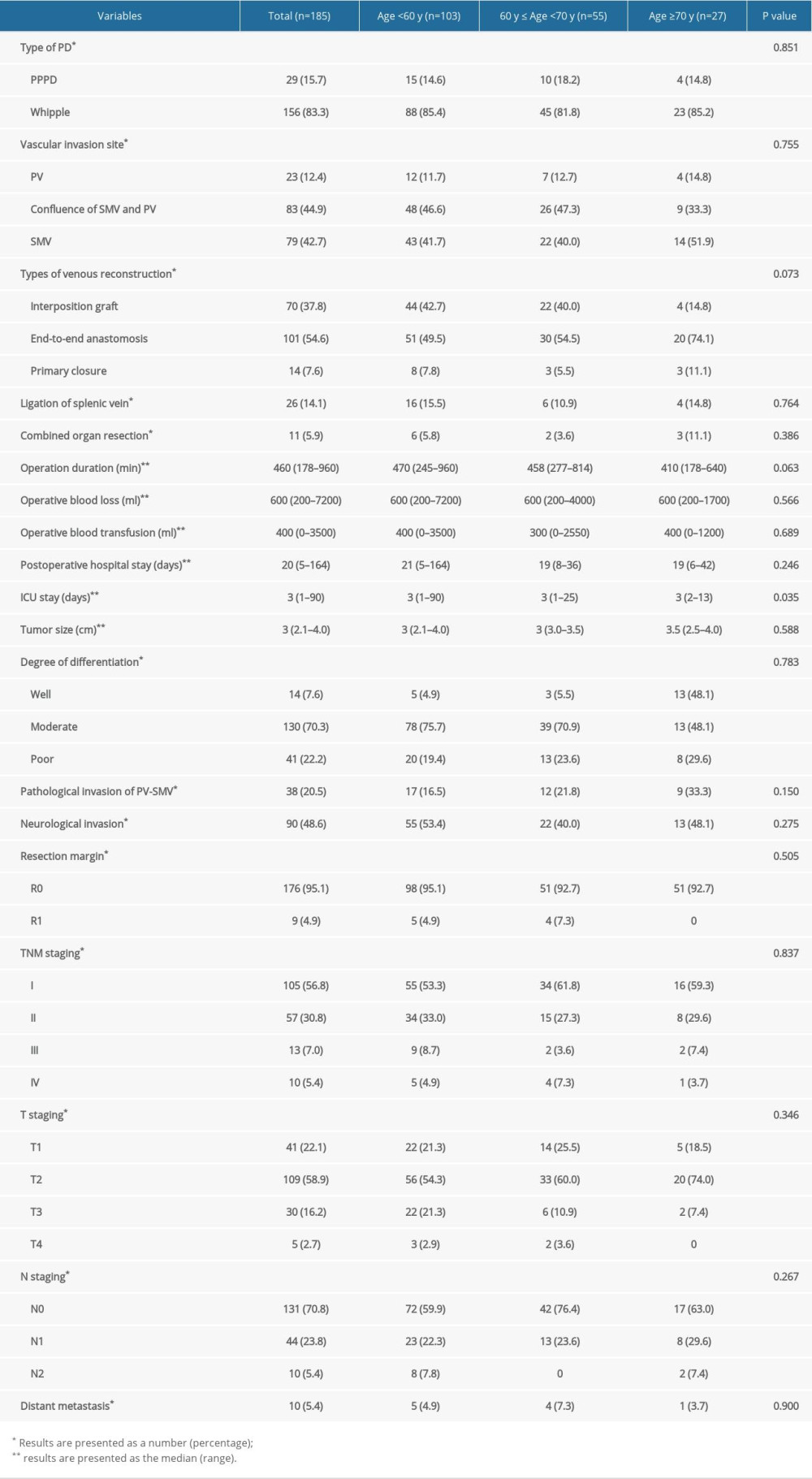 Table 2. Perioperative and pathologic characteristics of the PDAC patients who underwent PDR according to age.
Table 2. Perioperative and pathologic characteristics of the PDAC patients who underwent PDR according to age.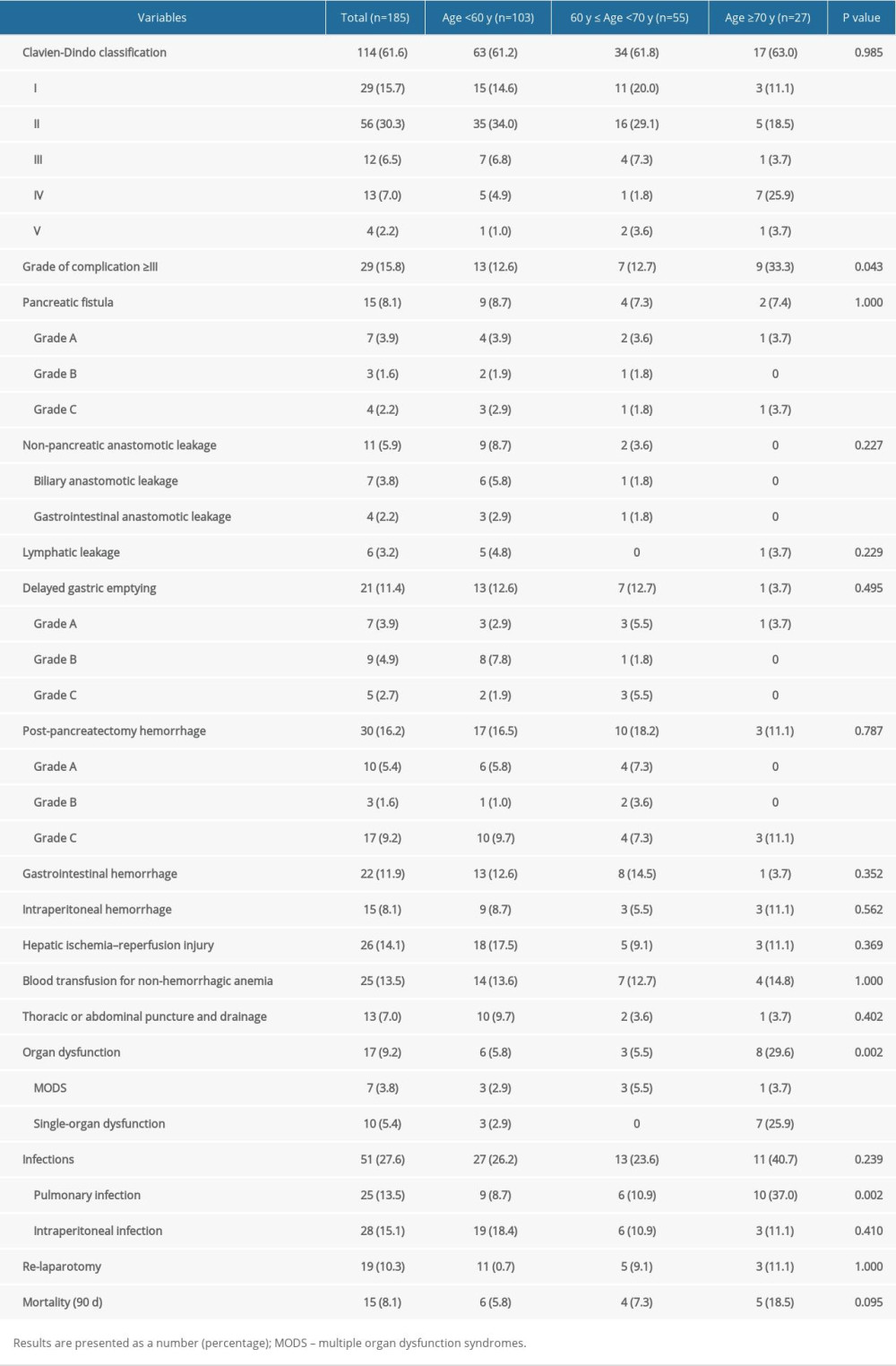 Table 3. Postoperative complications of stays the PDAC patients who underwent PDR according to age.
Table 3. Postoperative complications of stays the PDAC patients who underwent PDR according to age.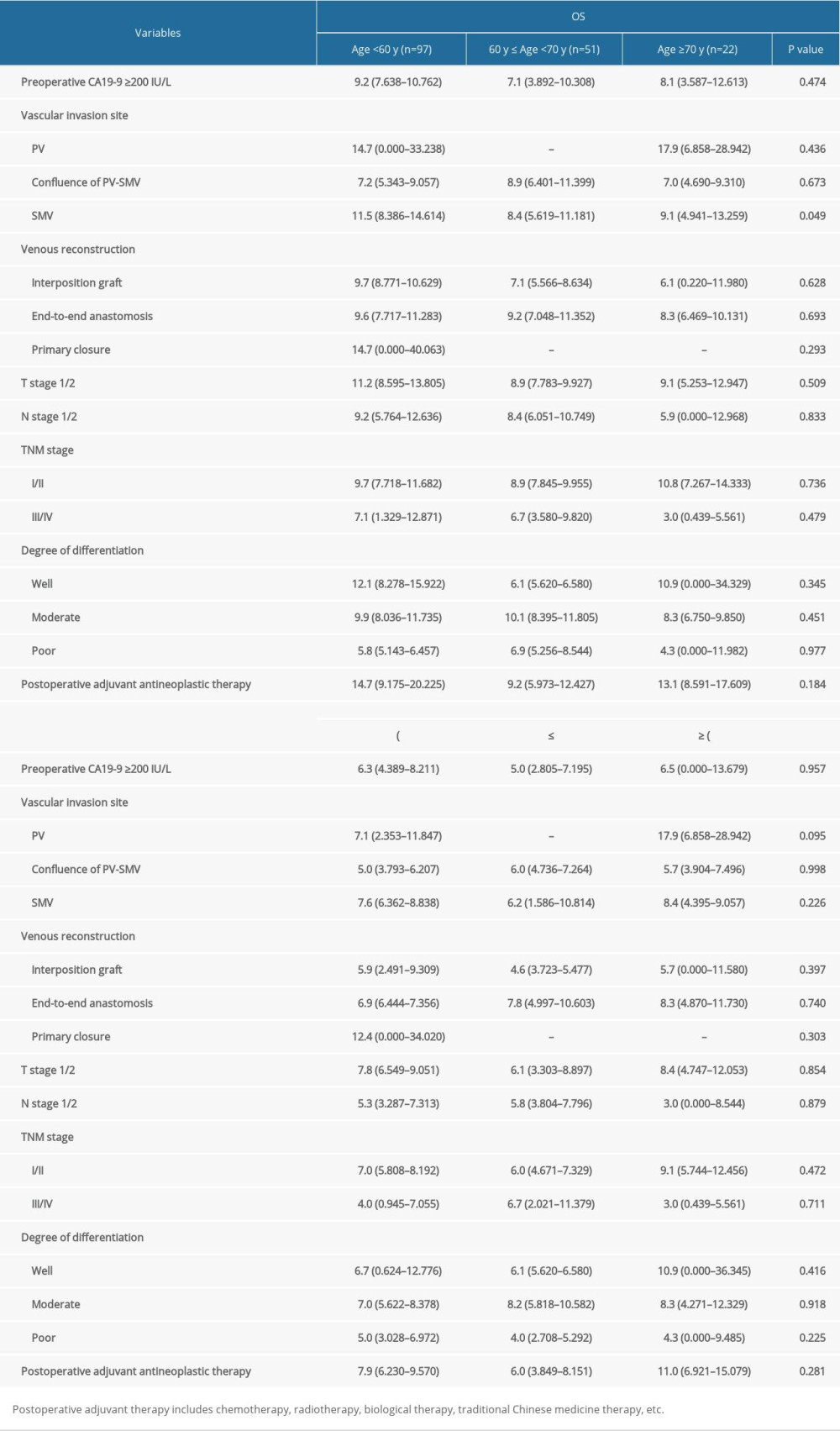 Table 4. Analysis of the OS and PFS of PDAC patients who underwent PDR according to age.
Table 4. Analysis of the OS and PFS of PDAC patients who underwent PDR according to age.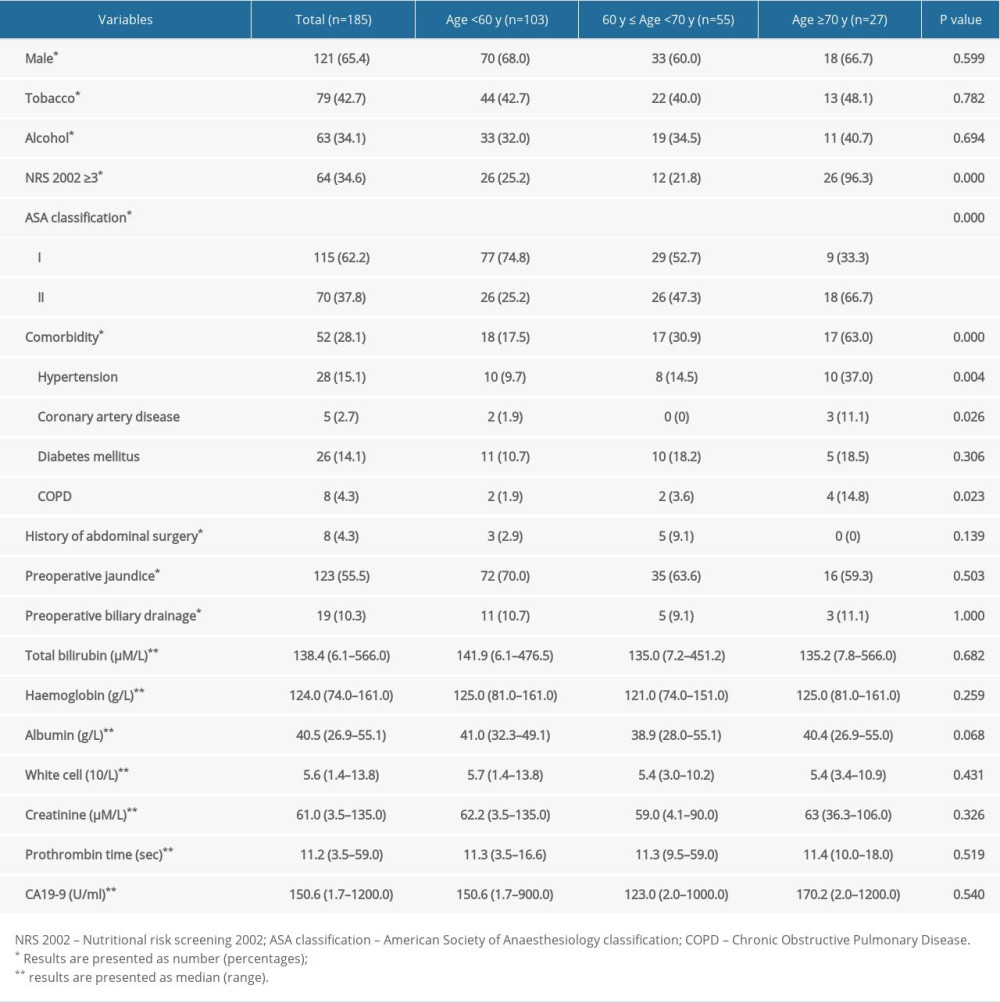 Table 1. Comparison the demographic and clinical characteristics of the PDAC patients who underwent PDR according to age.
Table 1. Comparison the demographic and clinical characteristics of the PDAC patients who underwent PDR according to age.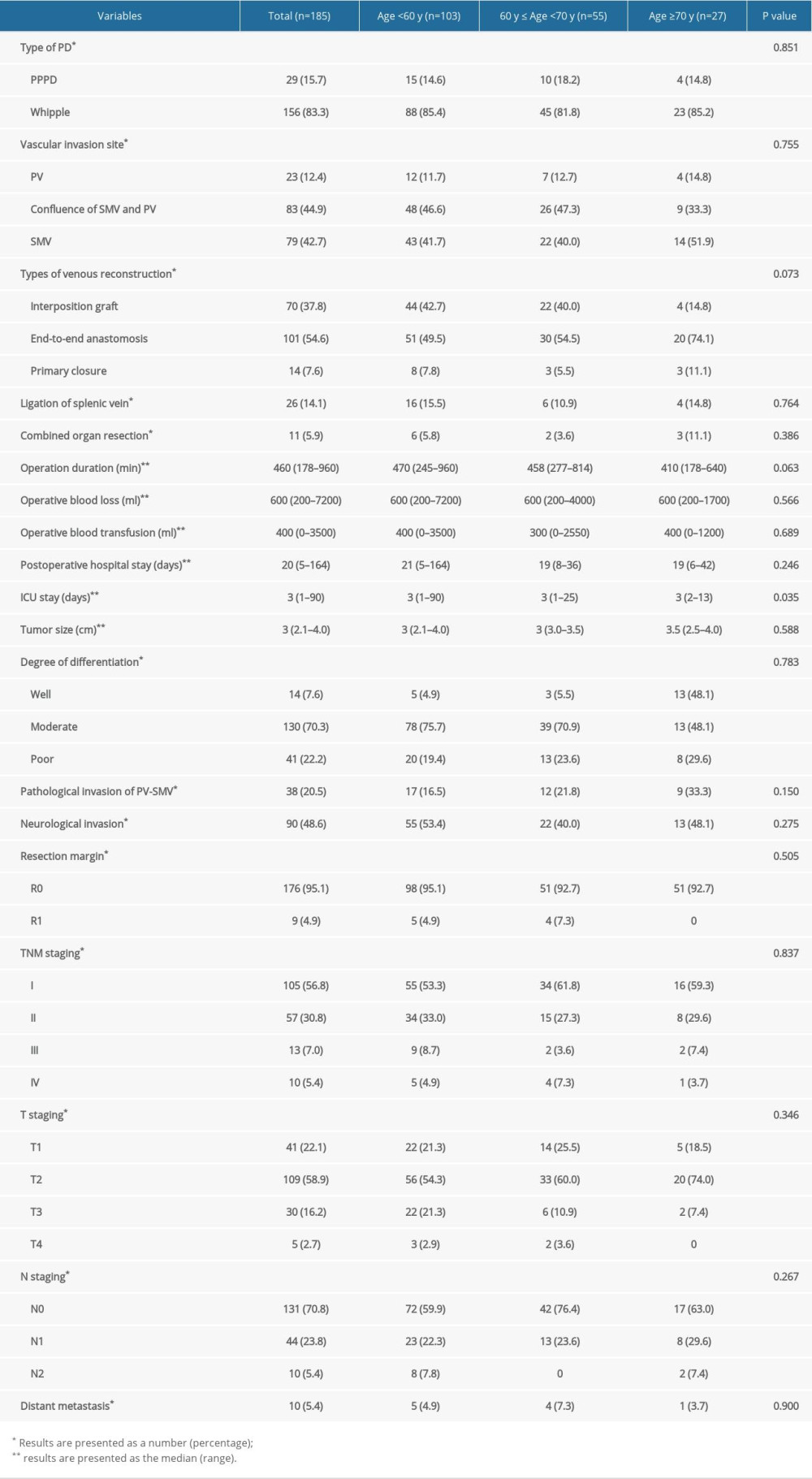 Table 2. Perioperative and pathologic characteristics of the PDAC patients who underwent PDR according to age.
Table 2. Perioperative and pathologic characteristics of the PDAC patients who underwent PDR according to age.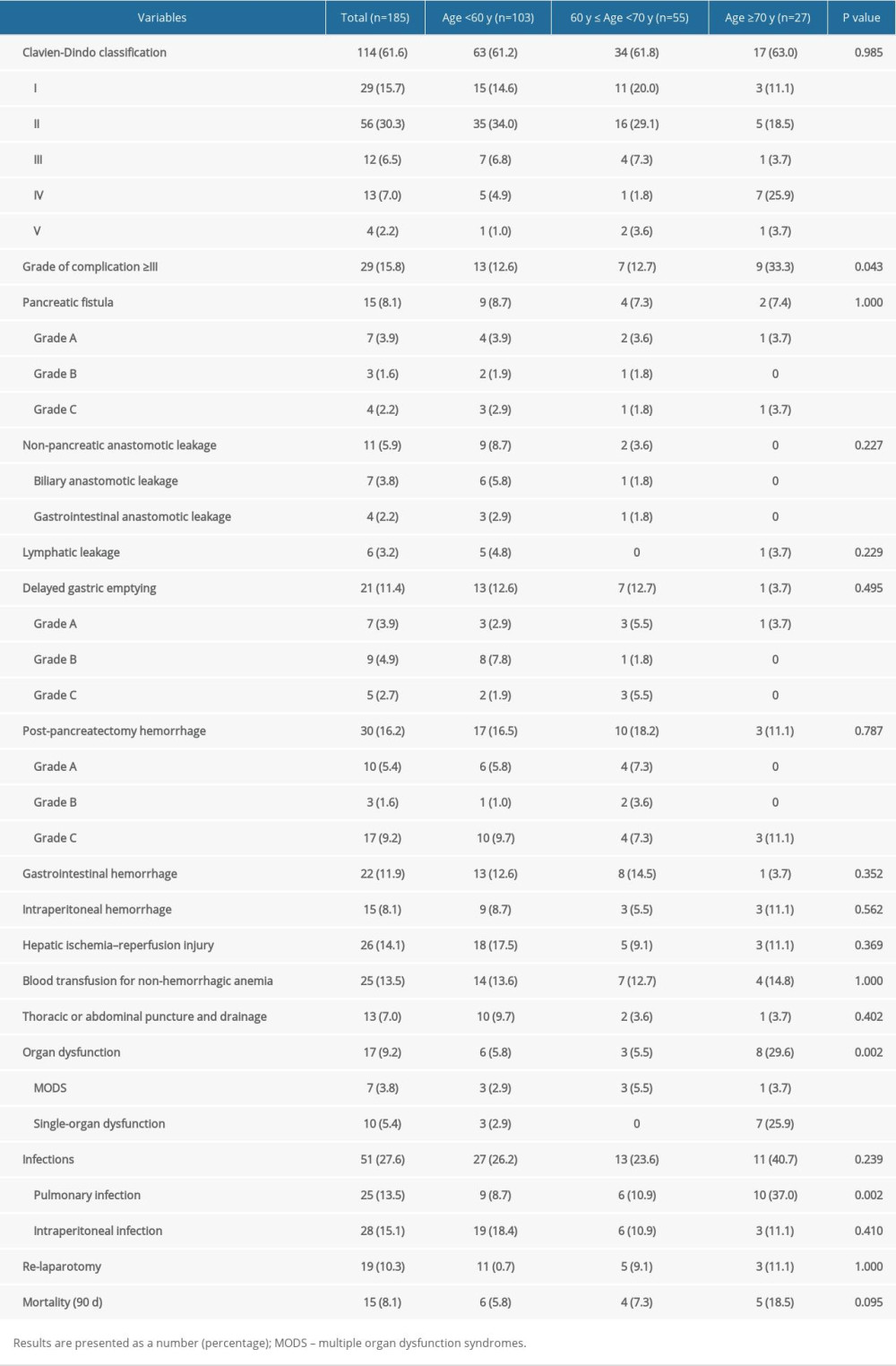 Table 3. Postoperative complications of stays the PDAC patients who underwent PDR according to age.
Table 3. Postoperative complications of stays the PDAC patients who underwent PDR according to age.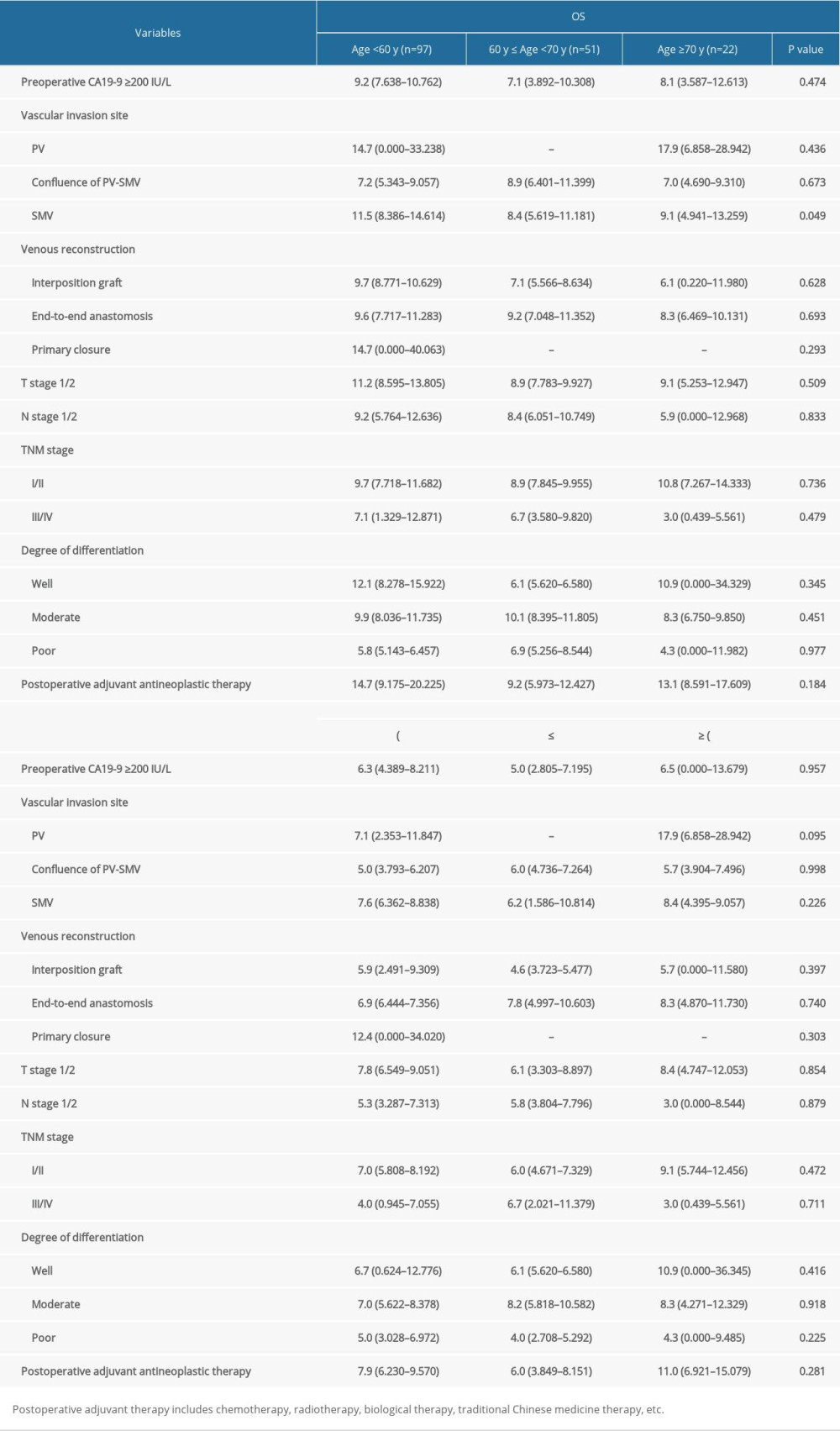 Table 4. Analysis of the OS and PFS of PDAC patients who underwent PDR according to age.
Table 4. Analysis of the OS and PFS of PDAC patients who underwent PDR according to age. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952