18 March 2024: Clinical Research
Association of T Cell Subsets and Platelet/Lymphocyte Ratio with Long-Term Complications in Kidney Transplant Recipients
Yun Yang1ABCDEFG, Jie-Hui Chen1BCDE, Shu-Xiao Zhang1BCDE, Sheng-Lang Zhu1ADEF*, Hengmei Zhu12AEFGDOI: 10.12659/MSM.942324
Med Sci Monit 2024; 30:e942324
Abstract
BACKGROUND: Infection and chronic rejection remain major issues for kidney transplant recipients (KTRs). The present study aimed to explore the association of CD4+/CD8+ T cell ratio (CD4+/CD8+) and platelet/lymphocyte ratio (PLR) with long-term infection and chronic renal insufficiency in KTRs.
MATERIAL AND METHODS: KTRs admitted to a single hospital from June 2014 to December 2021 were divided into infected (164) and non-infected (107) groups based on clinical data. The levels of CD4+/CD8+, PLR, neutrophil/lymphocyte ratio (NLR), and C-reactive Protein (CRP) in KTRs with long-term infection, and their correlation with chronic kidney insufficiency, were analyzed. Survival analysis was used to evaluate the risk factors for long-term infection and chronic kidney insufficiency.
RESULTS: Spearman correlation analysis showed that chronic kidney insufficiency was positively correlated with PLR, and negatively correlated with CRP and CD4+/CD8+ (P<0.05). PLR was positively correlated with CRP, procalcitonin, erythrocyte sedimentation rate, and NLR, but negatively with CD4+/CD8+. CD4+/CD8+ was correlated with CRP, NLR, and PLR (P<0.05). Survival analysis and survival curves showed that PLR and CD4+/CD8+ were risk factors for long-term infection and chronic kidney insufficiency in KTRs (P<0.05).
CONCLUSIONS: CD4+/CD8+ and PLR were associated with long-term complications, and were risk factors for long-term infection and chronic kidney insufficiency in KTRs.
Keywords: CD4-CD8 Ratio, Kidney Transplantation, Lymphocyte Count, Neutrophils, Platelet Count, Renal Insufficiency, Chronic, transplant recipients
Introduction
In light of the continuous improvement of the technical and perioperative management of kidney transplantation and the application of new immunosuppressants, kidney transplantation has become the best kidney replacement therapy for patients with end-stage renal disease, and has greatly improved the survival of patients with uremia [1]. However, infection and chronic rejection remain major issues for kidney transplant recipients (KTRs) and nephrologists. At present, most studies still focus on early infection and acute rejection in the perioperative period of kidney transplantation [2–4], and few studies exist on long-term complications of KTRs, such as predictors of long-term infection or chronic renal failure. As markers of circulating immune system components, T cell subsets can reflect the immune status of KTRs. A large number of studies have shown that the levels of CD4+ T cells and CD8+ T cells play important roles in infection and acute rejection in the perioperative period of kidney transplantation. This period has always been characterized by difficulty, and is a hotspot of organ transplantation research [5–8]. The derivative indexes platelet/lymphocyte ratio (PLR) and neutrophil/lymphocyte ratio (NLR) in the peripheral blood cell count, which can reflect the immune-inflammatory state of patients with chronic kidney disease, have been reported in multiple studies [9–14], but have been reported less often as markers in long-term chronic renal insufficiency in KTRs.
Therefore, the purpose of the present study was to investigate the relationship between T cell subsets and PLR in long-term infection and chronic renal insufficiency in KTRs. By providing new clinical evidence that could be used for the prevention and treatment of long-term complications in KTRs, the lifespan of a transplanted kidney could be extended, improving the quality of life for the patients.
Material and Methods
STUDY POPULATION:
The clinical data for kidney transplantation patients who were hospitalized in Huazhong University of Science and Technology Union Shenzhen Hospital (Nanshan Hospital) from June 2014 to December 2021 for more than half a year were analyzed retrospectively. The glomerular filtration rate (GFR) was calculated from the formula provided by the C16 000 biochemical instrument (Abbott, USA). The patients were divided into an infected group and a non-infected group, according to whether they were diagnosed with an infection during hospitalization. In the present study, long-term infection refers to acute infections diagnosed through medical records, clinical evaluations, and antibiotic prescriptions, excluding chronic infections such as hepatitis B, hepatitis C, and tuberculosis. Kidney insufficiency is defined as chronic kidney disease (CKD) stage 3 that is evident 6 months after transplantation, regardless of renal imaging changes. Inclusion criteria were: 1) patients who received kidney transplantation over 6 months and for whom the concentration of anti-rejection drugs was stable and within the standard range [15]; 2) adults (over 18 years old) with complete clinical data. Exclusion criteria were: patients with malignant tumors, severe hematological diseases, severe immune deficiency diseases, severe liver diseases, thyroid diseases, major trauma or surgery, and patients who underwent dialysis again after kidney transplantation. All the patients signed informed consent forms. This study has been approved by the hospital ethics committee [Application ID: KY-2021-066-01].
DETECTION INDEXES AND METHODS: COLLECTION OF CLINICAL DATA:
By querying the KTRs who met the standards and were hospitalized in our hospital from June 2014 to December 2021, the general clinical data and laboratory test indexes were obtained. These included sex, age, time of kidney transplantation, NLR, PLR, hemoglobin (HB), CRP, erythrocyte sedimentation rate (ESR), uric acid, creatinine, GFR, serum albumin (ALB), CD4+ T cells, CD8+ T cells, and CD4+/CD8+ ratio.
DETECTION INDEXES AND METHODS: DETECTION OF SERUM INDEXES:
Upon admittance, a complete blood count, which included evaluation of leukocytes, neutrophils, hemoglobin, lymphocytes, and platelets, and biochemical indexes such as creatinine, uric acid, GFR, and ALB were detected using venous blood. The NLR was calculated as the ratio of neutrophils to lymphocytes and the PLR was calculated as the ratio of platelets to lymphocytes. The percentage of T cell subsets such as CD4+ T cells and CD8+ T cells and the ratio of CD4+ T cells to CD8+ T cells were detected by flow cytometry.
On the day of admission, 3 mL of venous blood was taken from each patient. The supernatant was tested after centrifugation. Measurement of neutrophils, platelets, and lymphocytes was conducted with a fully automated blood cell analyzer [Heizenmekang XN9000, Japan], and the NLR and PLR ratios were calculated. CRP concentration in the serum was determined by a specific protein analyzer [CSC Bio Aristo, China]. An automatic chemiluminescence detector [New industry MAGLUMI 4000 PLus, China] was used to determine the procalcitonin concentration level. An automatic biochemical analyzer [Abbott C16 000, USA] was used to detect renal liver function and biochemical indexes.
Detection Indexes and Methods: Stages of Chronic Kidney Disease [16–17]
The estimated glomerular filtration rate (eGFR) was computed utilizing the creatinine equation from the Chronic Kidney Disease Epidemiology Collaboration. The patients were classified into 5 stages of CKD based on their eGFR: CKD stage1, GFR ≥90 mL/min; CKD stage 2, 90 mL/min >GFR ≥60 mL/min; CKD stage 3, 60 mL/min >GFR ≥30 mL/min; CKD stage 4, 30 mL/min >GFR ≥150 mL/min, CKD stage 5, GFR<15 mL/min.
STATISTICAL ANALYSIS:
SPSS 20.0 software (Chicago, USA) was used for statistical analysis. The normal measurement data were expressed by mean±standard deviation (χ̄±s), using an independent sample test, and skewed data were expressed as median and quartile, and analyzed by rank U test. Quantitative data were expressed as the number of cases and percentage, and were compared using a χ2 test. Spearman correlation analysis was conducted for the correlation of circulating immune-inflammatory indexes to long-term infection and CKD in KTRs.
Results
COMPARISON OF GENERAL CLINICAL DATA FOR KTRS:
A total of 271 hospitalized KTRs were included in this study, of which 164 KTRs had long-term infection (60.52%). There were 94 male patients (57.32%), which was a significantly higher number than female patients (P=0.015). However, no statistically significant difference was detected for age, kidney transplantation time, hemoglobin, ALB, serum creatinine, and GFR between the 2 groups (P>0.05). Demographic data for the 2 studied groups are shown in Table 1.
COMPARISON OF CIRCULATING IMMUNE-INFLAMMATORY INDEXES BETWEEN THE 2 KTR GROUPS:
Univariate analysis showed that there were significant differences in general immune-inflammatory indexes of CRP, ESR, procalcitonin, NLR, PLR, CD4+, CD8+, and CD4+/CD8+ ratio between the 2 groups (all P<0.05). The levels of CRP, ESR, procalcitonin, NLR, PLR, and CD8+ cell count were higher in the infected group than in the non-infected group. However, the CD4+ count and the CD4+/CD8+ ratio were lower in the infected group than in the non-infected group. The results of the laboratory tests are shown in Table 2.
Spearman Correlation Analysis of Circulating Immune-Inflammatory Indexes and Long-Term Infection and Chronic Kidney Insufficiency in KTRs
CRP, procalcitonin, ESR, NLR, and PLR were positively correlated with long-term infection in KTRs (P < 0.05), while blood uric acid and CD4+/CD8+ ratio were negatively correlated with long-term infection in KTRs (P<0.05). The results also showed that long-term renal insufficiency was positively correlated with ESR, uric acid, and PLR, and negatively correlated with CRP and CD4+/CD8+ ratio (P<0.05). PLR was positively correlated with CRP, procalcitonin, ESR, and NLR; and negatively correlated with CD4+/CD8+ ratio (P<0.05). CD4+/CD8+ ratio was negatively correlated with CRP, NLR, and PLR (P<0.05). All of these results are depicted in Table 3.
ADJUSTED COX PROPORTIONAL HAZARDS MODEL OF LONG-TERM INFECTION AND CHRONIC KIDNEY INSUFFICIENCY IN KTRS:
Predictive factors for long-term infection and chronic kidney insufficiency were evaluated using a Cox proportional hazards model, and the results are shown in Tables 4 and 5. Predictive factors associated with both long-term infection and chronic kidney insufficiency risk in KTRs included age, PLR, and CD4+/CD8+ ratio (all P<0.05).
Kaplan-Meier Survival Analysis and Survival Curves Analyzing Associations Between CD4+/CD8+ Ratio, PLR, Long-Term Infection, and Chronic Kidney Insufficiency in KTRs
Kaplan-Meier survival curves estimating the risks of long-term infection and chronic kidney insufficiency in kidney transplant recipients are presented in Figures 1–4. The curves are stratified by median values of the CD4+/CD8+ ratio and PLR groups. Notably, the higher CD4+/CD8+ ratio and lower PLR groups demonstrated a significantly increased cumulative risk of long-term infection (all P<0.05).
Discussion
Due to the implantation of grafts and the use of immunosuppressants, even a half year after receiving renal transplantation and successfully transitioning to the stable stage, KTRs are still at risk of immune state imbalance [18]. At the same time, long-term infection and chronic rejection are the main long-term complications for KTRs [19–21]. Our retrospective observational study aimed to evaluate the role and clinical significance of CD4+/CD8+ ratio and PLR in the process of immune-inflammatory activation in KTRs.
T lymphocytes, including CD4+ T cells and CD8+ T cells, mainly exist in peripheral lymphoid tissue and blood. The ratio of the 2 cell types is about 2: 1, and CD4+ cells are integral in regulating the immune state in the human body [22]. Because immunosuppressants are used after kidney transplantation to prevent rejection, the occurrence of infection caused by bacteria, viruses, and eukaryotic pathogens after transplantation is greatly increased. This is often accompanied by changes in the levels of lymphocyte subsets, and these changes can be valuable for evaluating prognosis in KTRs [7,23,24]. In general, the CD4+/CD8+ T cell ratio contains information on CD4+ T cells and CD8+ T cells. Our study indicated that the ratio of CD4+/CD8+ T cells was negatively correlated with long-term infection and chronic kidney insufficiency in KTRs, and this correlation was statistically significant (respectively, r=−0.451,
As markers of new circulating blood cells, PLR and NLR include a variety of blood cell information, such as platelets, lymphocytes, and neutrophils. They have important clinical value in evaluating infection and inflammatory response. At the same time, they have a certain predictive value for the loss of kidney function, particularly in CKD patients treated with non-renal replacement therapy [10,12]. Our study showed that NLR had a strong correlation with long-term infection in KTRs (r=0.740,
In summary, it can be seen that CD4+/CD8+ ratio and PLR are related to long-term infection events and chronic decline of renal function after kidney transplantation. The present study also used survival analysis and survival curves to demonstrate that PLR is strongly correlated with long-term infection in KTRs (
Conclusions
Our study demonstrated that CD4+/CD8+ ratio and PLR were important risk factors for long-term infection in KTRs. They were also related to the progress of CKD in KTRs. Finally, they were also important for the prediction of long-term immune status in KTRs. Therefore, this study could have clinical application value in preventing long-term complications, and thereby improving the lifespan of transplanted kidneys and delaying the decline of transplanted kidney function. It also provided a certain reference value for the monitoring of immune status and long-term health education in KTRs.
There are various forms of long-term complications for KTRs, such as chronic kidney transplant failure and immune disorders caused by the use of immunosuppressants, including chronic rejection after kidney transplantation, chronic inflammatory infections, tumors, hematopoietic dysfunction, and others. In the follow-up to this study, multiple patients with tumors and polycythemia have been found. However, more research about the long-term complications in KTRs would be beneficial for patients and society.
Figures
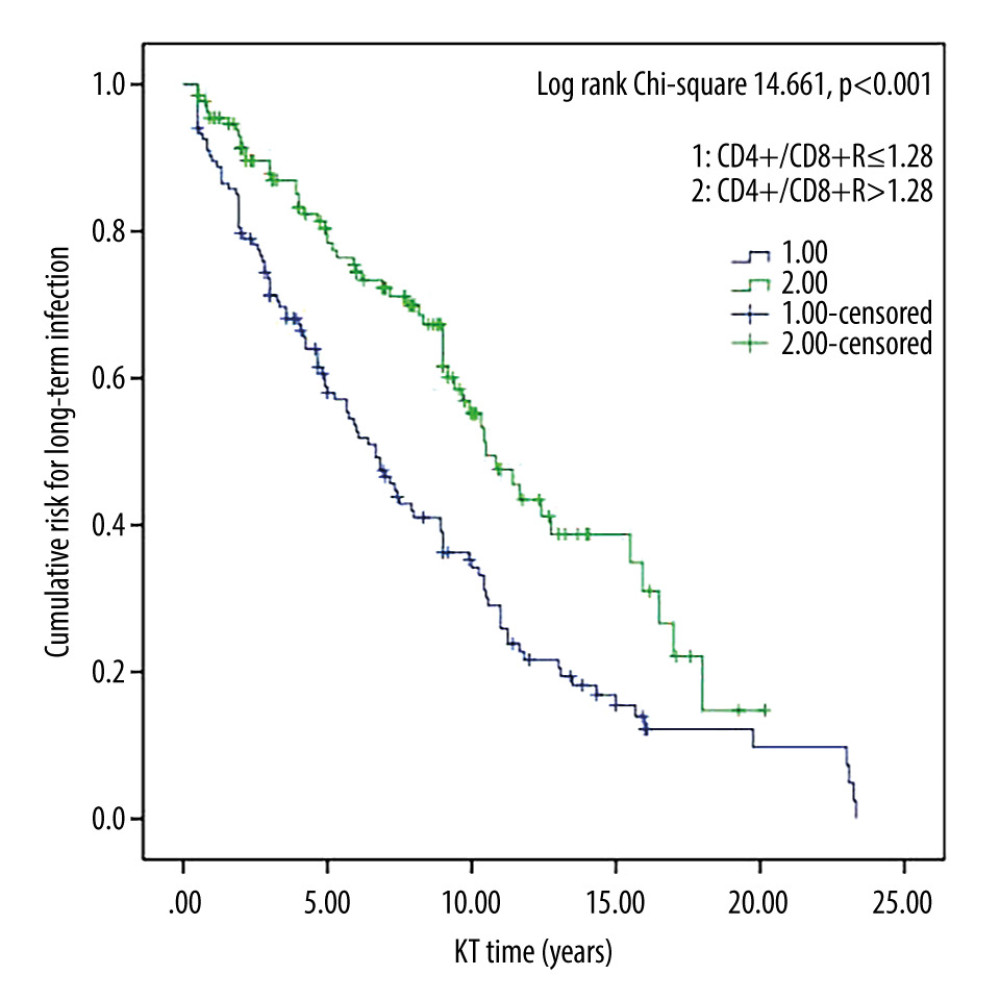 Figure 1. Survival curves for CD4+/CD8+ T cell ratio and long-term infection in kidney transplant recipients. Cumulative risk for long-term infection as a function of time (years) since kidney transplant. ThTsR – CD4+/CD8+ T-cell ratio; KT – kidney transplant.
Figure 1. Survival curves for CD4+/CD8+ T cell ratio and long-term infection in kidney transplant recipients. Cumulative risk for long-term infection as a function of time (years) since kidney transplant. ThTsR – CD4+/CD8+ T-cell ratio; KT – kidney transplant. 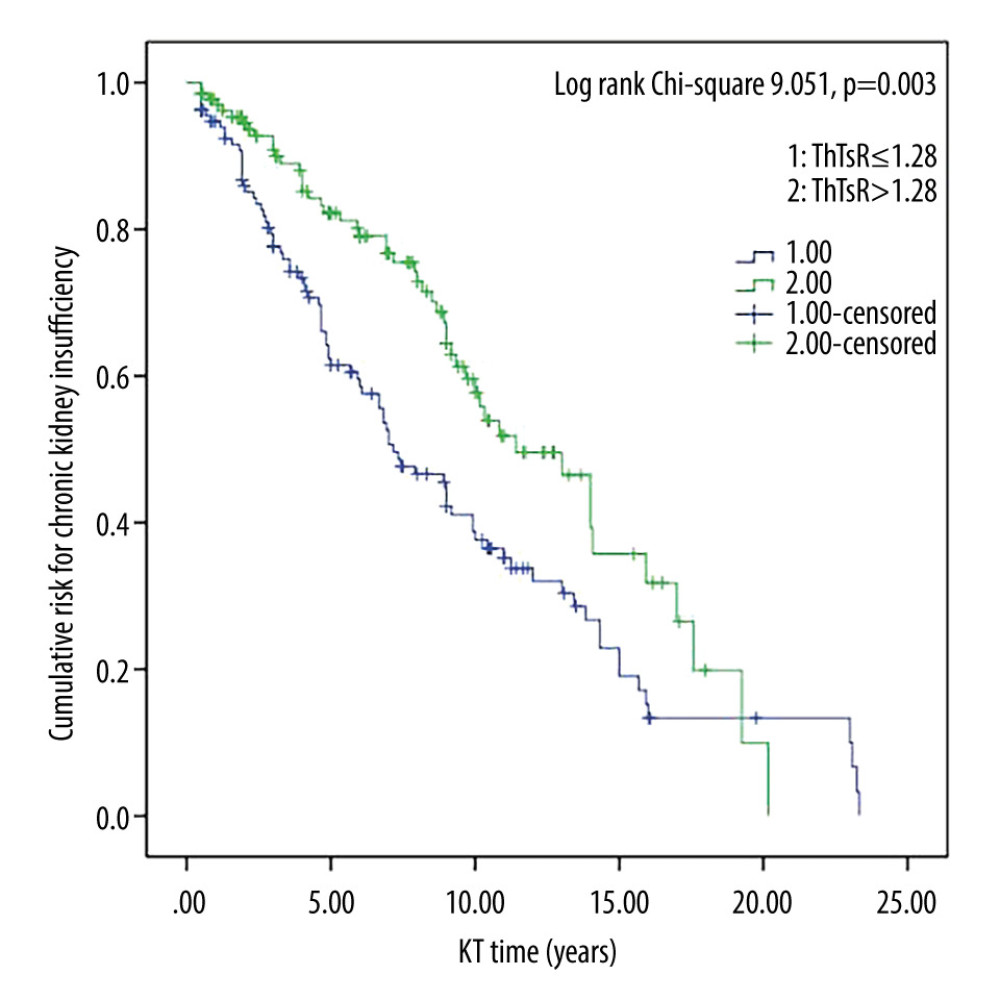 Figure 2. Survival curves for CD4+/CD8+ T-cell ratio and chronic kidney insufficiency in kidney transplant recipients. Cumulative risk for chronic kidney insufficiency as a function of time (years) since kidney transplant. ThTsR – CD4+/CD8+ T-cell ratio; KT – kidney transplant.
Figure 2. Survival curves for CD4+/CD8+ T-cell ratio and chronic kidney insufficiency in kidney transplant recipients. Cumulative risk for chronic kidney insufficiency as a function of time (years) since kidney transplant. ThTsR – CD4+/CD8+ T-cell ratio; KT – kidney transplant. 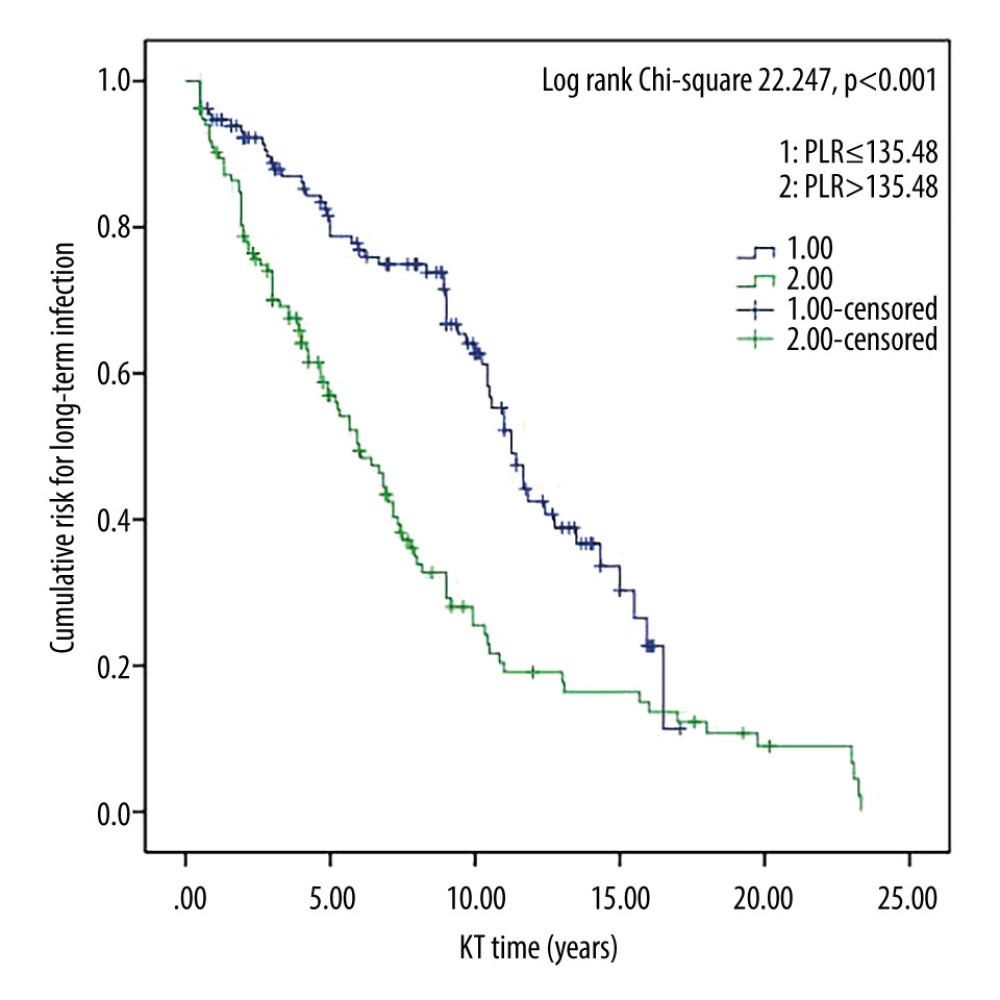 Figure 3. Survival curves for platelet/lymphocyte ratio and long-term infection in kidney transplant recipients. Cumulative risk for long-term infection as a function of time (years) since kidney transplant. PLR – platelet/lymphocyte ratio; KT – kidney transplant.
Figure 3. Survival curves for platelet/lymphocyte ratio and long-term infection in kidney transplant recipients. Cumulative risk for long-term infection as a function of time (years) since kidney transplant. PLR – platelet/lymphocyte ratio; KT – kidney transplant. 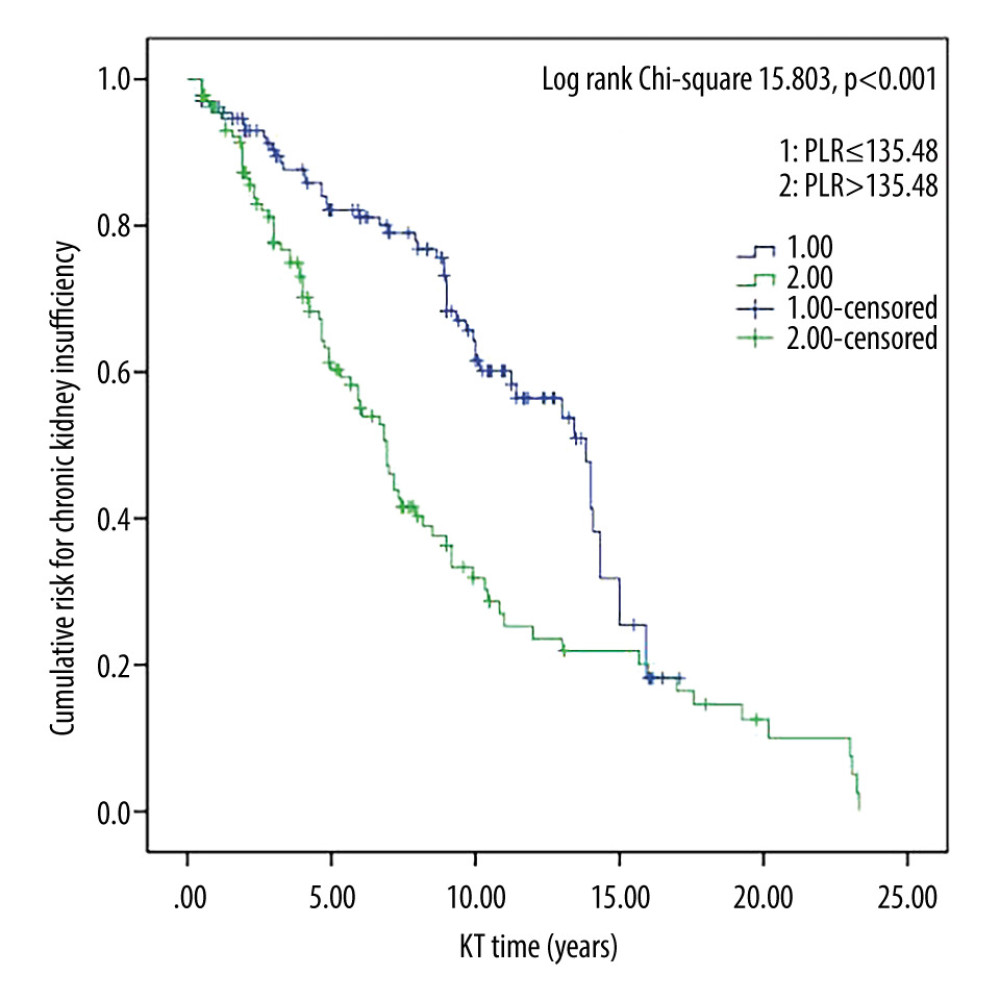 Figure 4. Survival curves for platelet/lymphocyte ratio and chronic kidney insufficiency in kidney transplant recipients. Cumulative risk for chronic kidney insufficiency as a function of time (years) since kidney transplant. PLR – platelet/lymphocyte ratio; KT – kidney transplant.
Figure 4. Survival curves for platelet/lymphocyte ratio and chronic kidney insufficiency in kidney transplant recipients. Cumulative risk for chronic kidney insufficiency as a function of time (years) since kidney transplant. PLR – platelet/lymphocyte ratio; KT – kidney transplant. Tables
Table 1. Comparison of general clinical data, between the non-infected group and the infected group of kidney transplant recipients.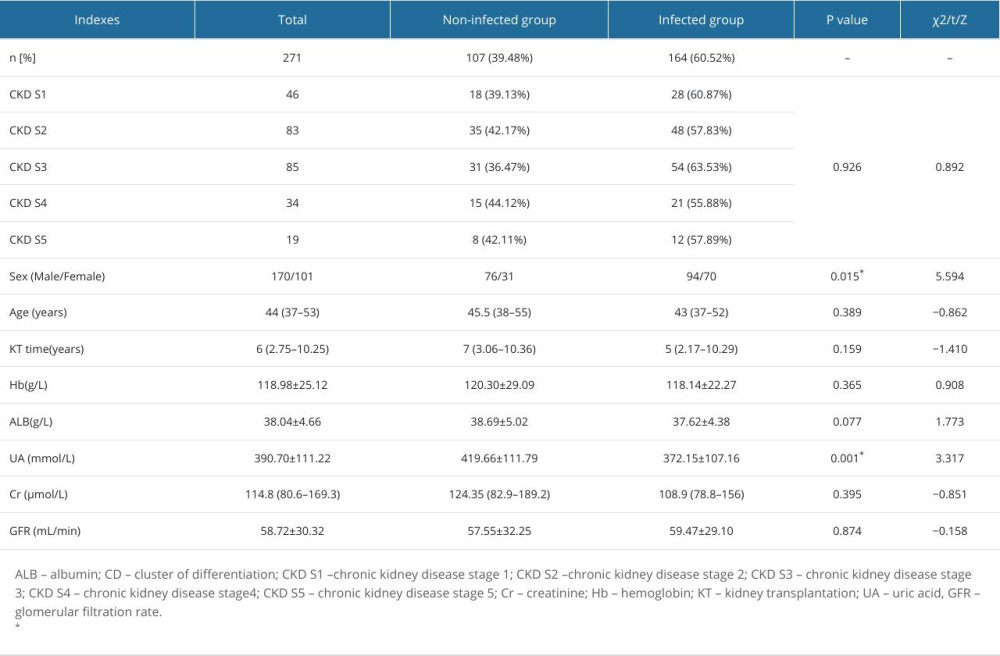 Table 2. Comparison of circulating immune-inflammatory indexes between the non-infected and infected groups of kidney transplant recipients.
Table 2. Comparison of circulating immune-inflammatory indexes between the non-infected and infected groups of kidney transplant recipients.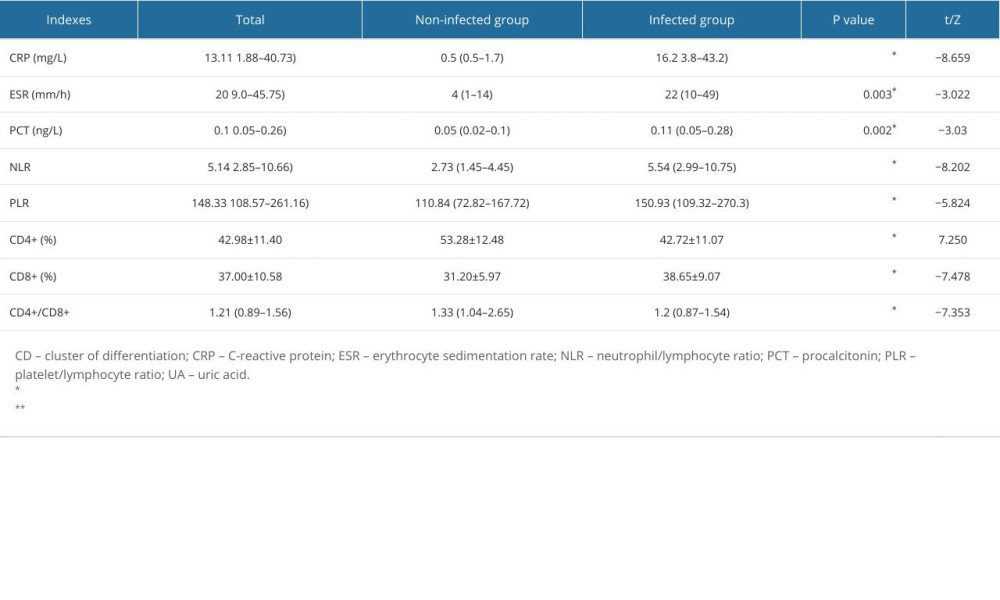 Table 3. Correlation of circulating immune-inflammatory indexes with long-term infection and chronic kidney disease in kidney transplant recipients.
Table 3. Correlation of circulating immune-inflammatory indexes with long-term infection and chronic kidney disease in kidney transplant recipients.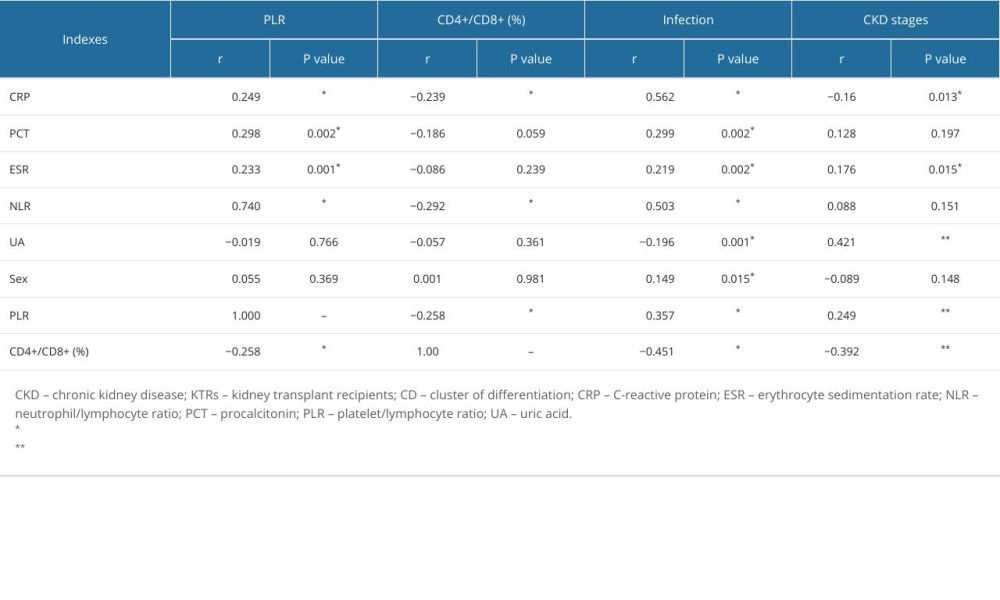 Table 4. Adjusted hazard ratios for risk of long-term infection in kidney transplant recipients.
Table 4. Adjusted hazard ratios for risk of long-term infection in kidney transplant recipients.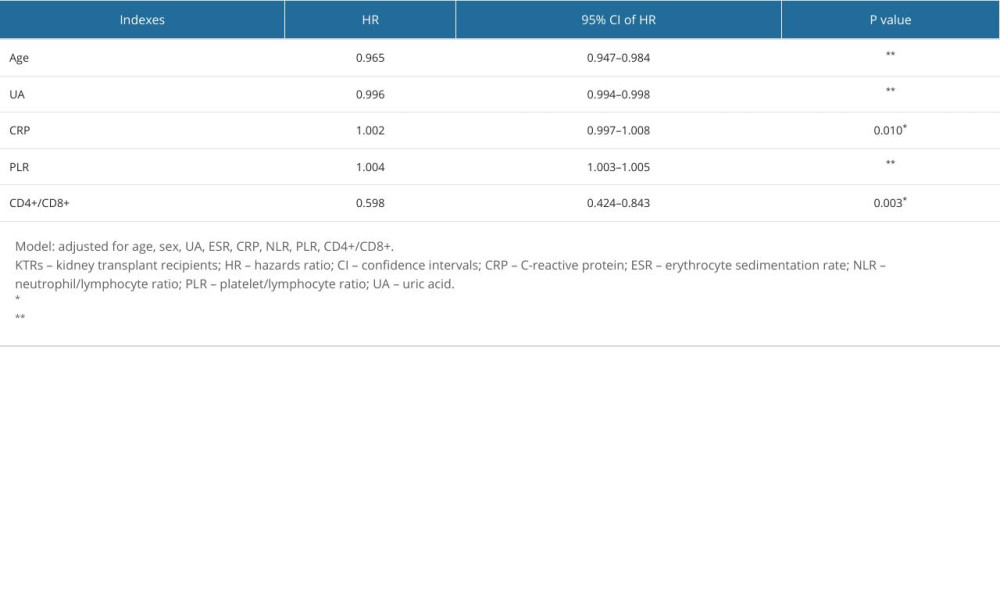 Table 5. Adjusted hazard ratios for risk of chronic kidney insufficiency in kidney transplant recipients.
Table 5. Adjusted hazard ratios for risk of chronic kidney insufficiency in kidney transplant recipients.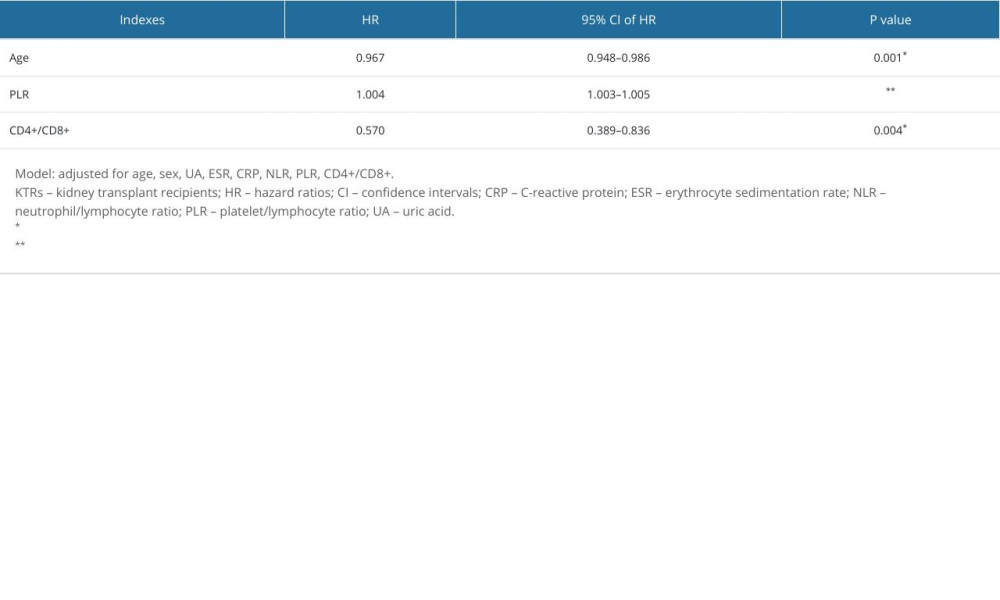
References
1. Chaudhry D, Chaudhry A, Peracha J, Survival for waitlisted kidney failure patients receiving transplantation versus remaining on waiting list: Systematic review and meta-analysis: BMJ, 2022; 376; e068769
2. Aikpokpo NV, Sharma A, Halawa A, Management of the failing kidney transplant: Challenges and solutions: Exp Clin Transplant, 2022; 20(5); 443-55
3. Oweira H, Ramouz A, Ghamarnejad O, Risk factors of rejection in renal transplant recipients: A narrative review: J Clin Med, 2022; 11(5); 1392
4. McDonald S, Russ G, Campbell S, Kidney transplant rejection in Australia and New Zealand: Relationships between rejection and graft outcome: Am J Transplant, 2007; 7(5); 1201-8
5. Perkey E, Maillard I, New insights into graft-versus-host disease and graft rejection: Annu Rev Pathol, 2018; 13; 219-45
6. Helanterä I, Mengel M, Revisiting acute T cell-mediated rejection in kidney allografts: Am J Transplant, 2022; 22(3); 681-82
7. Chandran S, Mannon RB, T cell-mediated rejection in kidney transplant recipients: The end(point) is also the beginning: Am J Transplant, 2022; 22(3); 683-84
8. Pickering H, Schaenman J, Rossetti M, T cell senescence and impaired CMV-specific response are associated with infection risk in kidney transplant recipients: Hum Immunol, 2022; 83(4); 273-80
9. Wheelock KM, Saulnier PJ, Tanamas SK, White blood cell fractions correlate with lesions of diabetic kidney disease and predict loss of kidney function in Type 2 diabetes: Nephrol Dial Transplant, 2018; 33(6); 1001-9
10. Zhao WM, Tao SM, Liu GL, Neutrophil-to-lymphocyte ratio in relation to the risk of all-cause mortality and cardiovascular events in patients with chronic kidney disease: A systematic review and meta-analysis: Ren Fail, 2020; 42(1); 1059-66
11. Brito GMC, Fontenele AMM, Carneiro ECRL, Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in nondialysis chronic kidney patients: Int J Inflam, 2021; 23; 6678960
12. Sevencan NO, Ozkan AE, Associations between neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, albuminuria and uric acid and the estimated glomerular filtration rate in hypertensive patients with chronic kidney disease stages 1–3: Arch Med Sci, 2019; 15(5); 1232-39
13. Siddiqui MA, Baskin E, Gülleroğlu KS, The role of platelet-lymphocyte ratio and neutrophil-lymphocyte ratio in predicting the delayed graft function in pediatric renal transplant patients: Exp Clin Transplant, 2022; 20(Suppl 3); 118-21
14. Ercan Emreol H, Büyükkaragöz B, Gönül İI, Value of neutrophil-lymphocyte and platelet-lymphocyte ratios in the evaluation of acute rejection and chronic allograft nephropathy in children with kidney transplantation: Exp Clin Transplant, 2022; 20(Suppl 3); 129-36
15. Oberbauer R, Bestard O, Furian L, Optimization of tacrolimus in kidney transplantation: New pharmacokinetic perspectives: Transplant Rev (Orlando), 2020; 34(2); 100531
16. Hall YN, Himmelfarb J, The CKD classification system in the precision medicine era: Clin J Am Soc Nephrol, 2017; 12; 346-48
17. Levey AS, Coresh J, Bolton K, K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification: Am J Kidney Dis, 2002; 39(2 Suppl 1); S1-266
18. Petrara MR, Serraino D, Di Bella C, Immune activation, immune senescence and levels of Epstein Barr Virus in kidney transplant patients: Impact of mTOR inhibitors: Cancer Lett, 2020; 469; 323-31
19. Faenko AP, Zulkarnaev AB, Fedilina VA, The long-term infective complications in patients after kidney transplantation and photopheresis: Urologia, 2018(5); 28-34
20. Fiorentino M, Pesce F, Schena A, Updates on urinary tract infections in kidney transplantation: J Nephrol, 2019; 32(5); 751-61
21. Kang SS, Park WY, Jin K, Characteristics of recipients with 10 or more years of allograft survival in deceased donor kidney transplantation: Transplant Proc, 2018; 50(4); 1013-17
22. Liu HC, Li PF, Wei ZP, Regulation of T cell differentiation and function by epigenetic modification enzymes: Semin Immunopathol, 2019; 41(3); 315-26
23. Shaw BI, Lee HJ, Chan C, Relationship between antithymocyte globulin, T cell phenotypes, and clinical outcomes in pediatric kidney transplantation: Am J Transplant, 2021; 21(2); 766-75
24. Franzese O, Mascali A, Capria A, Regulatory T cells in the immunodiagnosis and outcome of kidney allograft rejection: Clin Dev Immunol, 2013; 2013; 852395
Figures
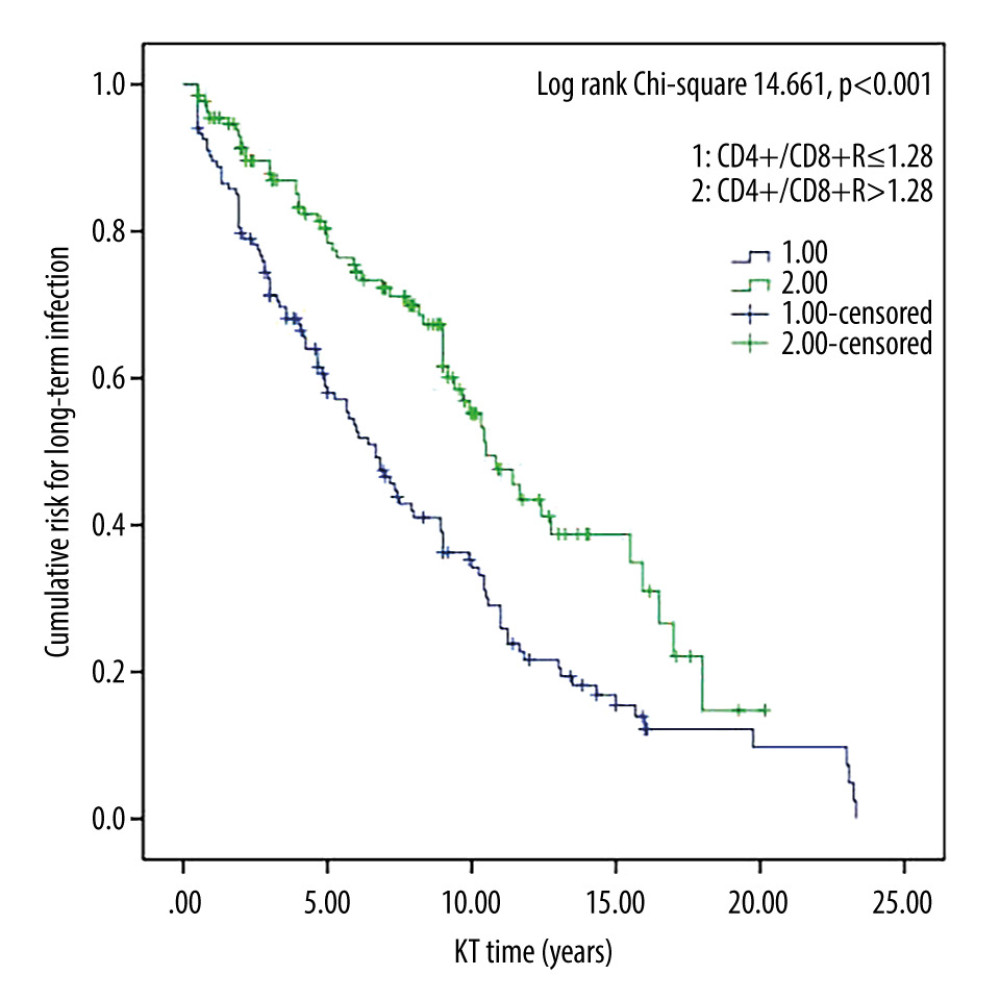 Figure 1. Survival curves for CD4+/CD8+ T cell ratio and long-term infection in kidney transplant recipients. Cumulative risk for long-term infection as a function of time (years) since kidney transplant. ThTsR – CD4+/CD8+ T-cell ratio; KT – kidney transplant.
Figure 1. Survival curves for CD4+/CD8+ T cell ratio and long-term infection in kidney transplant recipients. Cumulative risk for long-term infection as a function of time (years) since kidney transplant. ThTsR – CD4+/CD8+ T-cell ratio; KT – kidney transplant.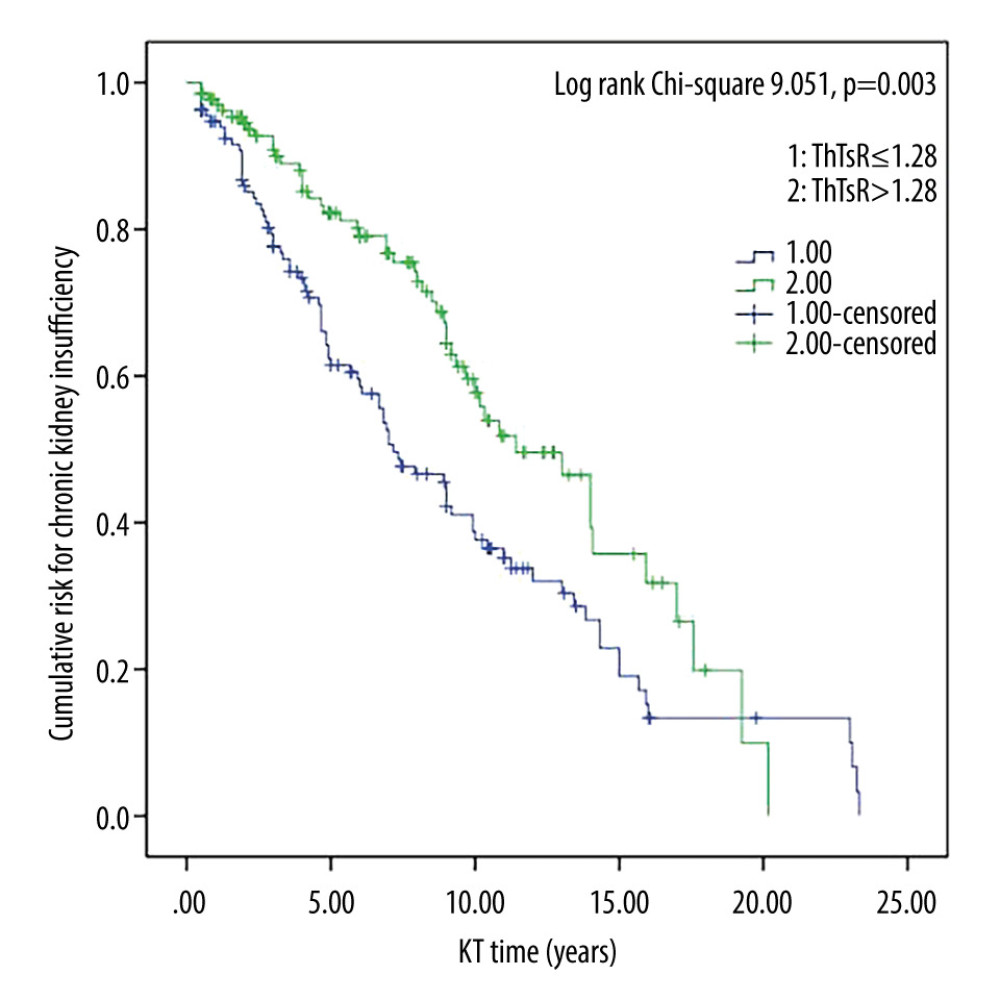 Figure 2. Survival curves for CD4+/CD8+ T-cell ratio and chronic kidney insufficiency in kidney transplant recipients. Cumulative risk for chronic kidney insufficiency as a function of time (years) since kidney transplant. ThTsR – CD4+/CD8+ T-cell ratio; KT – kidney transplant.
Figure 2. Survival curves for CD4+/CD8+ T-cell ratio and chronic kidney insufficiency in kidney transplant recipients. Cumulative risk for chronic kidney insufficiency as a function of time (years) since kidney transplant. ThTsR – CD4+/CD8+ T-cell ratio; KT – kidney transplant.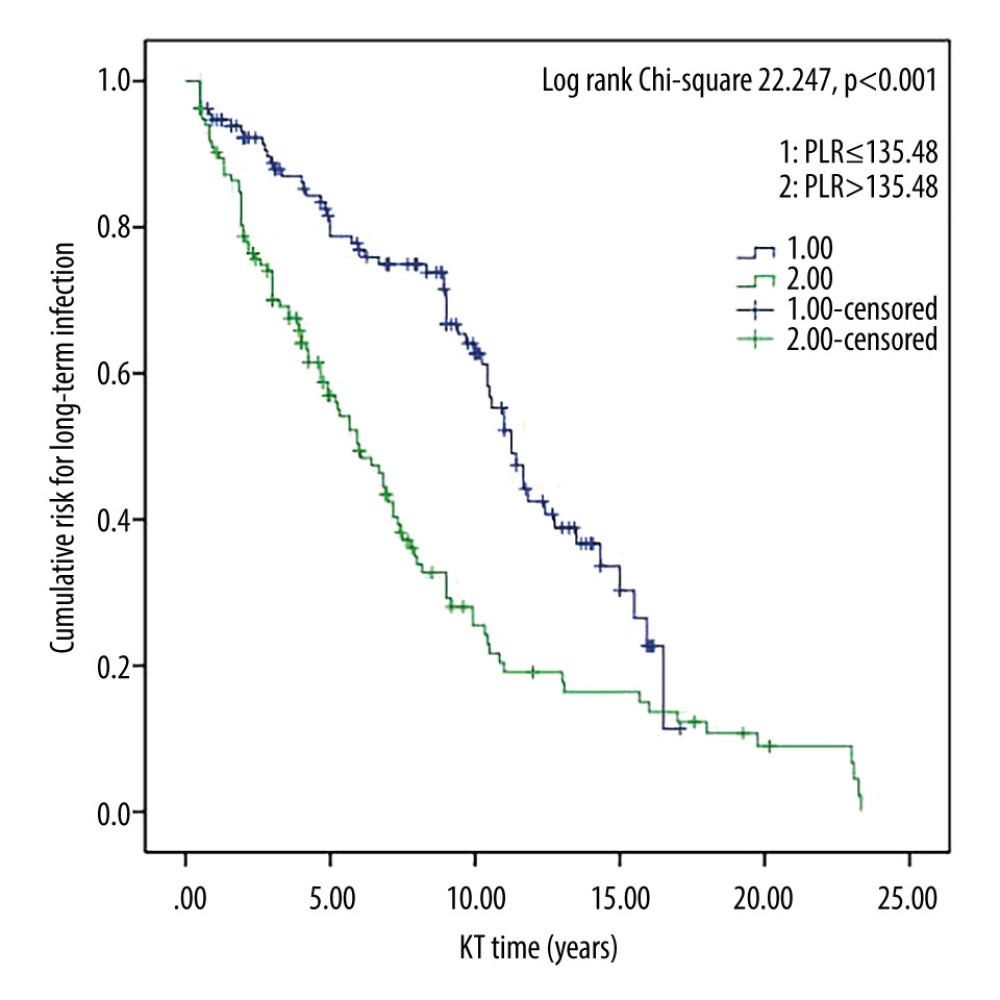 Figure 3. Survival curves for platelet/lymphocyte ratio and long-term infection in kidney transplant recipients. Cumulative risk for long-term infection as a function of time (years) since kidney transplant. PLR – platelet/lymphocyte ratio; KT – kidney transplant.
Figure 3. Survival curves for platelet/lymphocyte ratio and long-term infection in kidney transplant recipients. Cumulative risk for long-term infection as a function of time (years) since kidney transplant. PLR – platelet/lymphocyte ratio; KT – kidney transplant.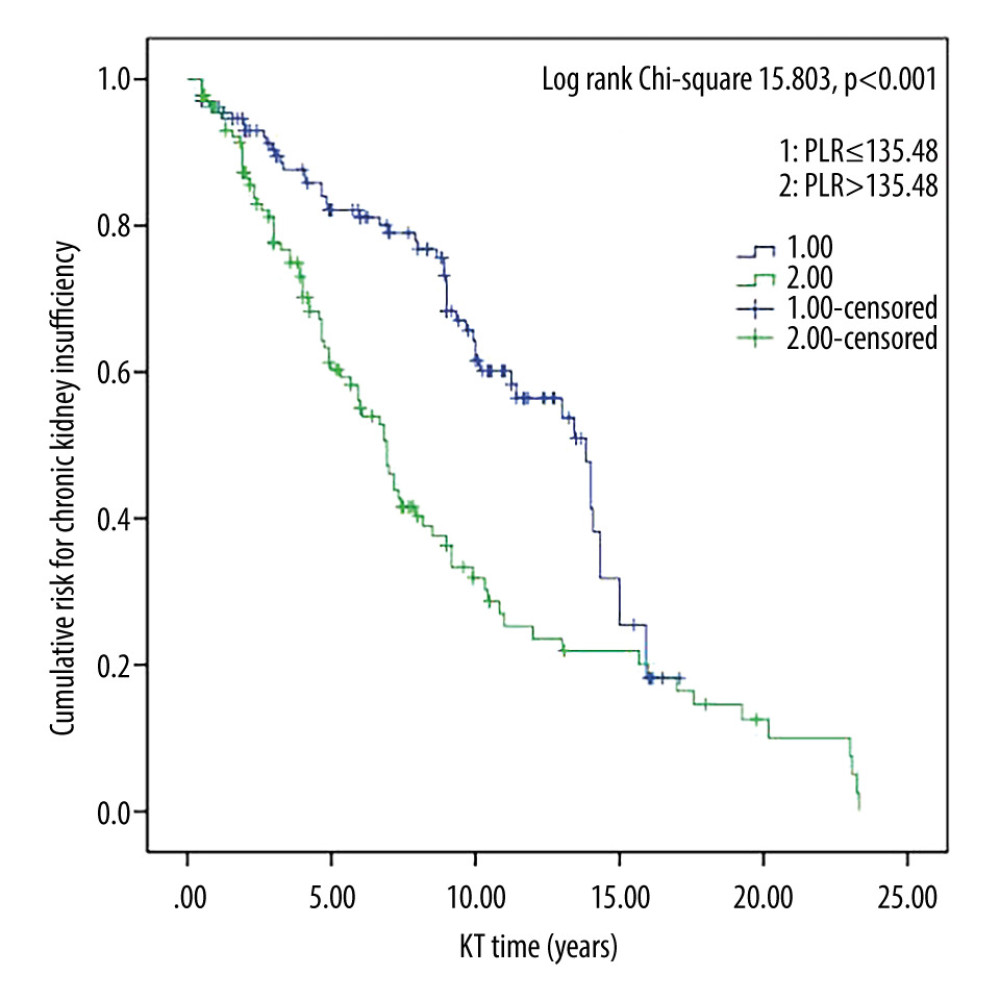 Figure 4. Survival curves for platelet/lymphocyte ratio and chronic kidney insufficiency in kidney transplant recipients. Cumulative risk for chronic kidney insufficiency as a function of time (years) since kidney transplant. PLR – platelet/lymphocyte ratio; KT – kidney transplant.
Figure 4. Survival curves for platelet/lymphocyte ratio and chronic kidney insufficiency in kidney transplant recipients. Cumulative risk for chronic kidney insufficiency as a function of time (years) since kidney transplant. PLR – platelet/lymphocyte ratio; KT – kidney transplant. Tables
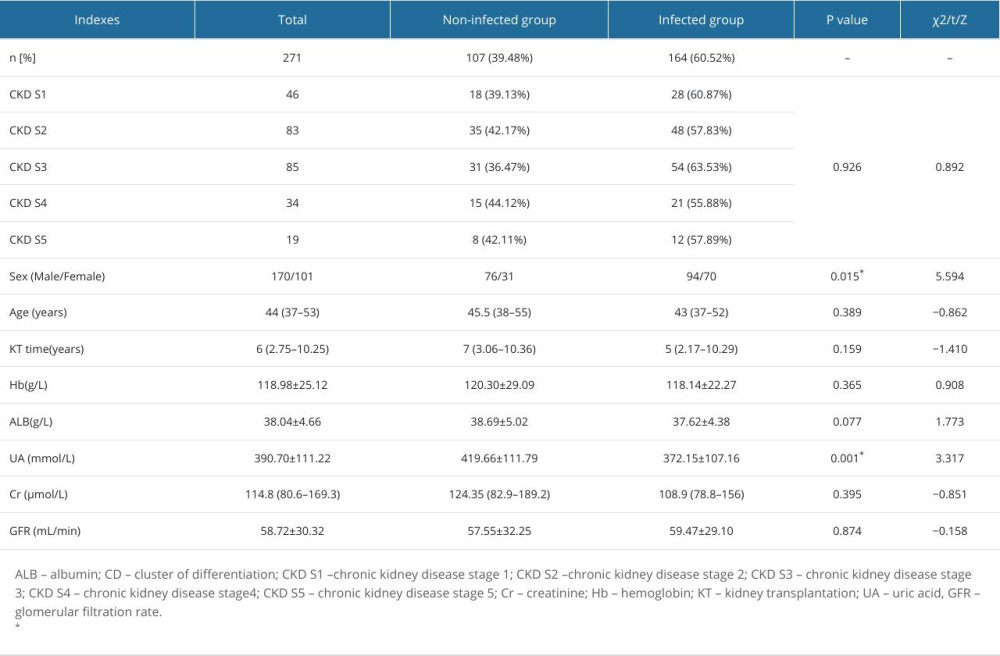 Table 1. Comparison of general clinical data, between the non-infected group and the infected group of kidney transplant recipients.
Table 1. Comparison of general clinical data, between the non-infected group and the infected group of kidney transplant recipients.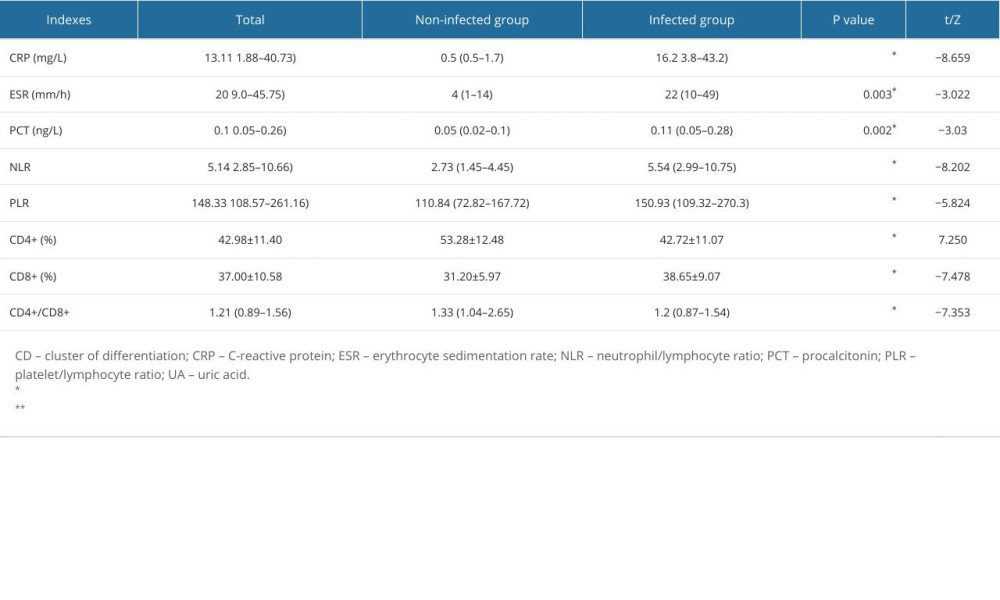 Table 2. Comparison of circulating immune-inflammatory indexes between the non-infected and infected groups of kidney transplant recipients.
Table 2. Comparison of circulating immune-inflammatory indexes between the non-infected and infected groups of kidney transplant recipients.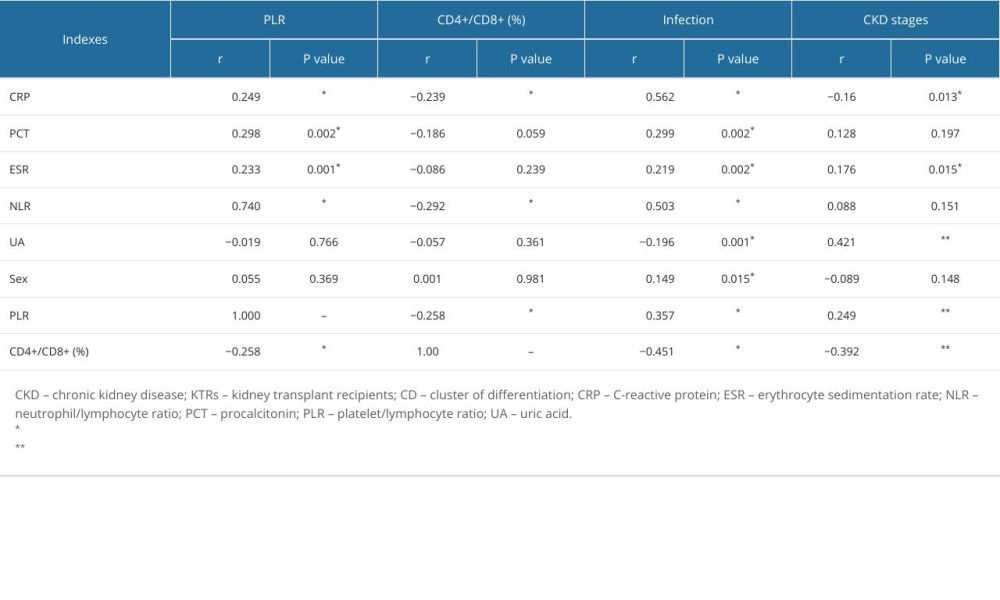 Table 3. Correlation of circulating immune-inflammatory indexes with long-term infection and chronic kidney disease in kidney transplant recipients.
Table 3. Correlation of circulating immune-inflammatory indexes with long-term infection and chronic kidney disease in kidney transplant recipients.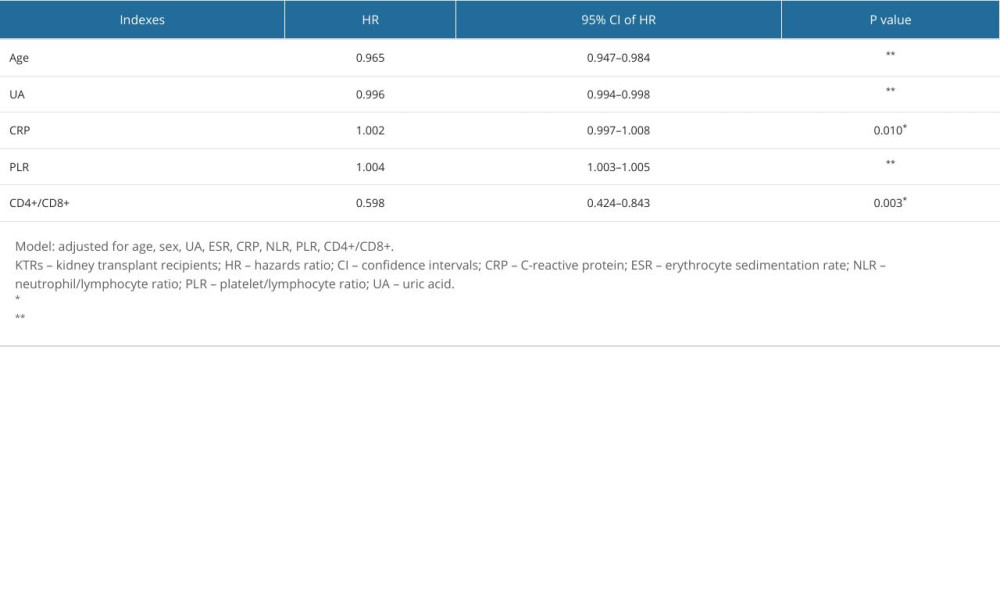 Table 4. Adjusted hazard ratios for risk of long-term infection in kidney transplant recipients.
Table 4. Adjusted hazard ratios for risk of long-term infection in kidney transplant recipients.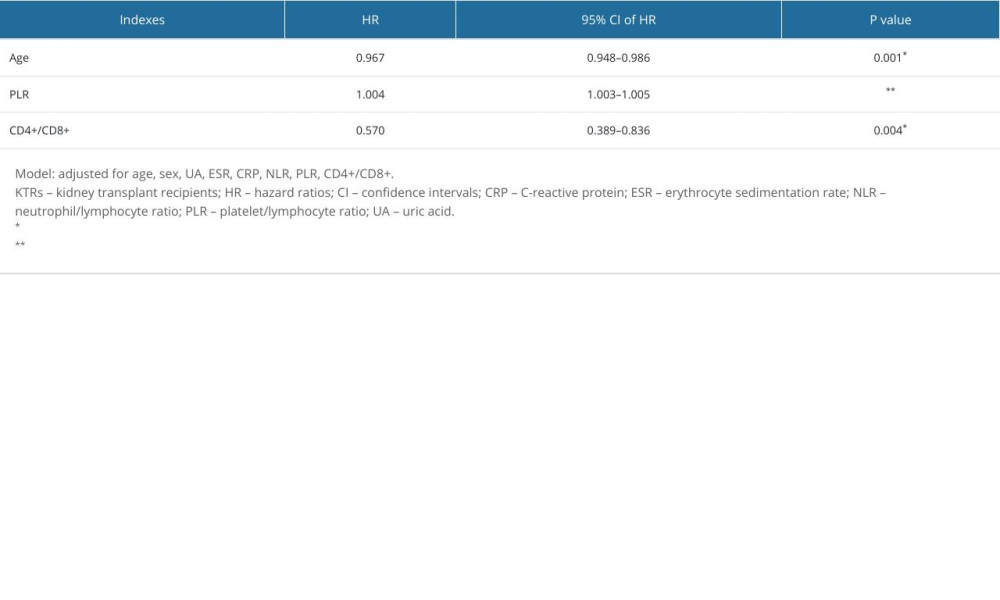 Table 5. Adjusted hazard ratios for risk of chronic kidney insufficiency in kidney transplant recipients.
Table 5. Adjusted hazard ratios for risk of chronic kidney insufficiency in kidney transplant recipients.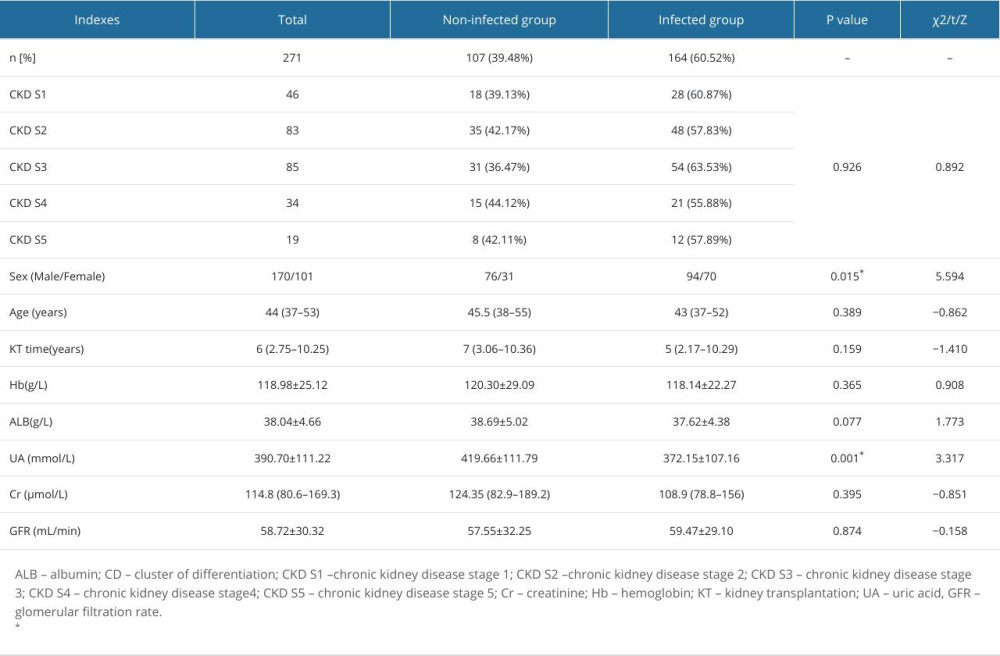 Table 1. Comparison of general clinical data, between the non-infected group and the infected group of kidney transplant recipients.
Table 1. Comparison of general clinical data, between the non-infected group and the infected group of kidney transplant recipients.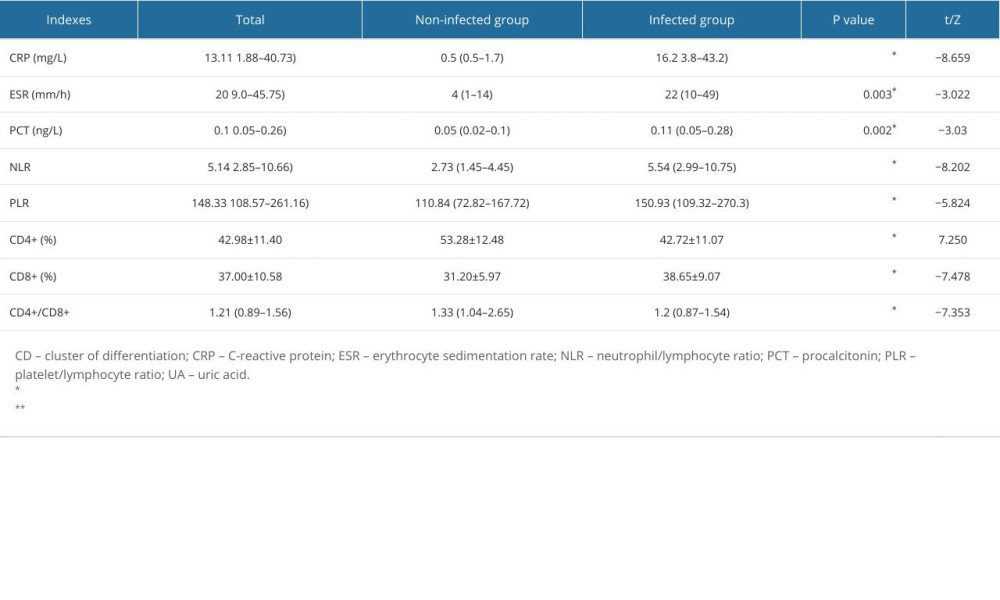 Table 2. Comparison of circulating immune-inflammatory indexes between the non-infected and infected groups of kidney transplant recipients.
Table 2. Comparison of circulating immune-inflammatory indexes between the non-infected and infected groups of kidney transplant recipients.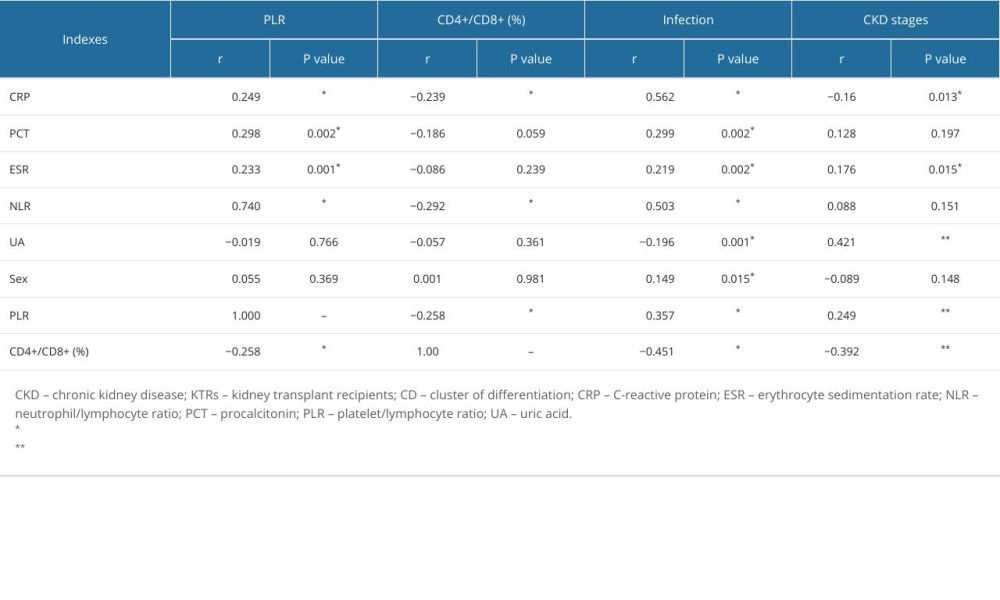 Table 3. Correlation of circulating immune-inflammatory indexes with long-term infection and chronic kidney disease in kidney transplant recipients.
Table 3. Correlation of circulating immune-inflammatory indexes with long-term infection and chronic kidney disease in kidney transplant recipients.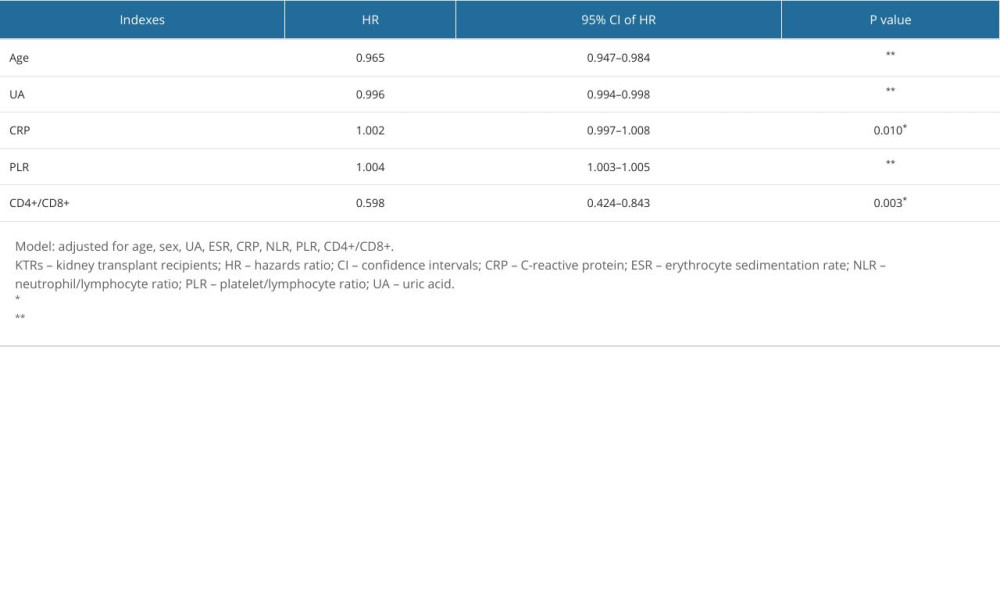 Table 4. Adjusted hazard ratios for risk of long-term infection in kidney transplant recipients.
Table 4. Adjusted hazard ratios for risk of long-term infection in kidney transplant recipients.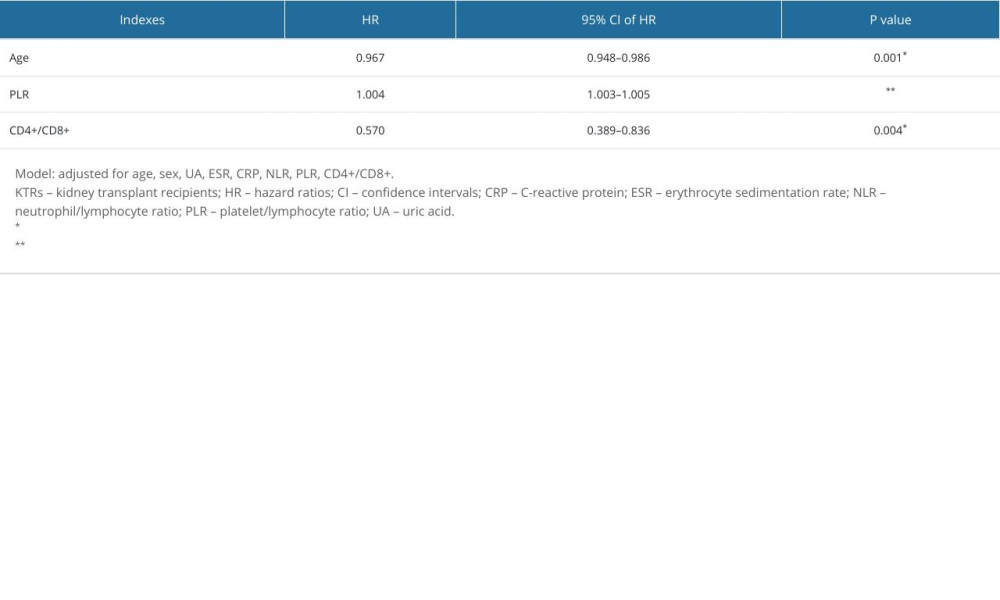 Table 5. Adjusted hazard ratios for risk of chronic kidney insufficiency in kidney transplant recipients.
Table 5. Adjusted hazard ratios for risk of chronic kidney insufficiency in kidney transplant recipients. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








