16 March 2024: Clinical Research
Retrospective Study to Compare the Effectiveness of Minimally Invasive Microscopic Unilateral Laminotomy with Microscopic Bilateral Laminotomy for Bilateral Decompression in the Early Postoperative Period in 142 Patients with Single-Level Lumbar Spinal Stenosis
Bülent Gülensoy1ABFG*, Serkan Şimşek2DEDOI: 10.12659/MSM.943815
Med Sci Monit 2024; 30:e943815
Abstract
BACKGROUND: We aimed to compare the effectiveness of microscopic unilateral laminotomy for bilateral decompression (ULBD) and microscopic bilateral laminotomy for bilateral decompression (BLBD) in the early postoperative period among patients with single-level lumbar spinal stenosis (LSS).
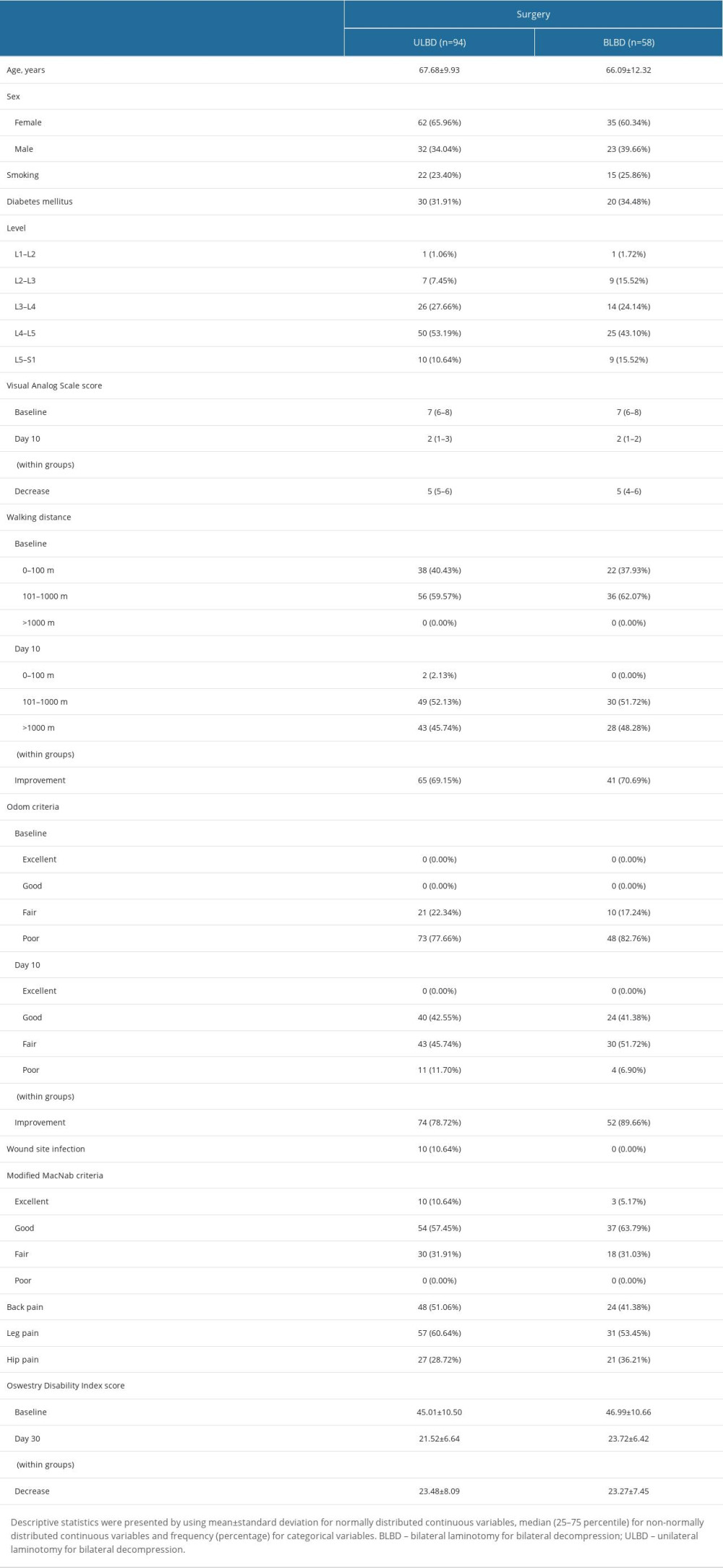
MATERIAL AND METHODS: A retrospective cohort study was conducted on patients with LSS who underwent ULBD or BLBD between January 2020 and December 2023, including 94 patients who underwent ULBD and 58 who underwent BLBD. Patient demographics, comorbidities, smoking status, and data related to LSS were reviewed. Preoperative and postoperative assessments on day 10 included back pain visual analog scale (VAS), walking distance, and Odom criteria. Disability was evaluated using the self-assessment Oswestry Disability Index (ODI) preoperatively and on day 30. Additionally, wound infection, postoperative modified MacNab criteria, and pain (back, leg, and hip) were recorded.
RESULTS: Age and sex were similar in the 2 groups. Both surgeries significantly reduced low back pain, increased walking distance, and improved Odom category on day 10, compared with baseline (P<0.001 for all). A significant decrease in 30-day ODI, compared with baseline, was observed in both groups (P<0.001 for both). The ULBD group had a significantly higher percentage of patients with wound infection (P=0.014); however, the ODI score among ULBD recipients was significantly lower (better) on day 30 (P=0.047).
CONCLUSIONS: ULBD may represent a less invasive, more effective, and safer surgical alternative than BLBD and classical laminectomy in patients with single-level LSS, but precautions are essential concerning wound infection.
Keywords: Lumbar Vertebrae, Spinal Canal, Spinal Stenosis
Introduction
Lumbar spinal stenosis (LSS) is a disabling spinal disease that causes low back pain, leg pain, and decreased quality of life [1]. Although there is no definitive information on the prevalence of LSS, it is estimated that approximately 103 million people have symptomatic LSS worldwide [2]. LSS is often based on facet joint growth, ligamentum flavum hypertrophy, disc degeneration, and osteophytes, which can lead to the narrowing of the spinal canal, lateral recess, and neuro-foramen, ultimately causing neurovascular compression [1,3–5].
The diagnosis of lumbar spinal stenosis can usually be made with a careful history and physical examination and is supported by imaging [2]. Diagnostic improvements have led to a higher frequency of LSS diagnosis, which has made LSS surgery the most frequently performed spinal surgery in recent years [1,3]. Surgery is performed in patients with prolonged symptoms who do not respond to conservative treatment [6]. For decompression, interventions such as total laminectomy, unilateral laminotomy, bilateral laminotomy, and open-door laminoplasty are used; however, there is no consensus on the optimal surgical procedure [1,7]. In theory, the optimal surgical procedure should provide maximum effect with minimal trauma and should not lead to complications [3]. Therefore, the primary goals of LSS surgery are to safeguard the nerve roots and medulla spinalis, limit postoperative morbidity and complications, and relieve symptoms, while minimizing tissue injury [3].
Compared with conventional laminectomy, the microscopic laminotomy procedure is a less invasive technique that can be used for the treatment of LSS [8]. Laminotomy can be performed unilaterally and bilaterally. Microscopic unilateral laminotomy for bilateral decompression (ULBD) is a minimally invasive technique that, in addition to treating symptoms and improving function, is suggested to shorten operating time, prevent surgical complications, and reduce instability by preserving the facet joints [9–11]. These claims have been substantiated by many studies showing that ULBD provides satisfactory symptomatic and functional improvement in the short, medium, and long term, with a low risk of complications in patients with LSS [12–14]. However, ULBT is described to be a difficult procedure, compared with bilateral laminotomy for bilateral decompression (BLBD), and has been demonstrated to prolong operating time, increase bleeding, and elevate risks for dural sac lesions [15–17]. Therefore, there is an ongoing debate regarding the utility of ULBD compared with that of BLBD; however, evidence is limited, indicating the need for comparative research focusing on these interventions.
Therefore, in this study, we aimed to compare the microscopic ULBD and BLBD procedures in terms of pain, functional outcomes, disability-related recovery, and other clinical parameters in the early postoperative period among patients with single-level LSS.
Material and Methods
ETHICS:
This study was approved by the local ethics committee, with the reference number E-53875521-050-21778, dated December 7, 2023. All procedures conducted were in accordance with the ethical standards of the institutional research committee and with the Helsinki declaration and its later amendments. All data were anonymized to maintain the privacy of all participants. Since the study was retrospective, the informed consent form was waived.
STUDY DESIGN AND PARTICIPANTS:
A retrospective cohort study was performed in patients with LSS who underwent surgery between January 2020 and December 2023 at the Department of Neurosurgery of Lokman Hekim University, Ankara, Turkey. The inclusion criteria were individuals undergoing either ULBD or BLBD procedures for LSS manifesting at a single vertebral level; age 18 years or older; patients presenting with symptoms indicative of neurogenic claudication or radiculopathy, supported by radiological evidence confirming degenerative LSS; and, to be deemed a candidate for surgery, patients should have demonstrated a lack of responsiveness to conservative treatment for a minimum of 3 months.
Exclusion criteria were a history of prior spinal surgery, those with documented psychiatric disorders, individuals experiencing ambulatory challenges attributable to orthopedic issues, and patients presenting with disc prolapse, degenerative listhesis, posterior arthrosis, scoliosis, or facet joint cyst concomitant with LSS. Furthermore, cases with inflammation-inducing disease or malignancy, as well as those with known disorders potentially influencing wound healing (excluding diabetes) were excluded.
DATA COLLECTION AND DEFINITIONS:
The patients’ age, sex and comorbidity information, smoking status, and preoperative, operative, and postoperative information regarding spinal stenosis were collected retrospectively from the hospital computerized database and patient charts.
CONSERVATIVE TREATMENT:
Patients presenting symptoms indicative of LSS underwent a comprehensive neurological examination, and preoperative radiological assessments were conducted for all patients, using plain X-ray, magnetic resonance imaging (MRI), and computed tomography (CT) imaging. The specific level of spinal stenosis for each patient was ascertained based on the imaging results. Conservative management, incorporating nonsteroidal anti-inflammatory drugs, activity limitations, and physical therapies, was initiated for patients with LSS confirmed through imaging. Those individuals who did not exhibit a positive response to a minimum of 3 months of conservative treatment were scheduled for surgical intervention [3,8].
PREOPERATIVE MANAGEMENT OF LSS AND INSTRUMENTS:
Prior to surgery, a standardized neurological and clinical evaluation was administered to all patients, assessing the severity of back pain, general symptoms, walking distance, and disability. Back pain severity was quantified using a self-assessment 10-point visual analog scale (VAS). The patients were categorized based on walking distance into 3 groups: 0–100 m, 101–1000 m, and >1000 m. Following the Odom criteria, patients were classified into 4 groups: excellent, good, fair, and poor [18]. Preoperative disability was assessed using the Oswestry Disability Index (ODI), which is a self-report method, as previously described [19].
SURGICAL PROCEDURES:
Patients underwent either ULBD or BLBD and were grouped with respect to the surgical process. Surgical intervention was deemed necessary in cases where there was enduring radicular leg pain, neurological deficits, or neurogenic intermittent claudication resistant to a minimum of 3 months of conservative treatment. This decision was based on the presence of moderate to severe canal stenosis, as indicated by MRI findings.
Following induction of general endotracheal anesthesia, all patients underwent standard microsurgical procedures at our hospital, with the utilization of equipment from Carl Zeiss Co. (Oberkochen, Germany). The surgeries were performed with the patients in the prone position [8,20]. In all procedures, the use of high-speed burrs, Kerrison rongeurs, and speculum-type retractors was standard practice. Both the ULBD and BLBD procedures used the undercut technique, involving minimal resection of the facet joints. Subsequent to the surgeries, postoperative CT imaging was conducted for all patients to evaluate decompression.
In the BLBD procedure, resection involved the lower section of the cranial lamina and minimally the upper part of the underlying lamina. Subsequently, flavectomy was performed to expose the spinal canal. Resection of the medial side of the facet joint was conducted to alleviate pressure within the lateral recess. Preservation encompassed the spinous process, supra- and interspinous ligaments, and a substantial portion of the lamina [8,20].
In ULBD, the procedure involved ipsilateral laminotomy, during which the lower section of the spinous process was cut using a high-speed milling cutter. Subsequent to ipsilateral decompression, the microscopic image was angled, and the contralateral ligamentum flavum and medial aspects of the contralateral facet joints were resected to achieve contralateral decompression [8].
POSTOPERATIVE ANALYSES:
The patients’ back pain VAS scores, walking distance ratios, Odom criteria, modified MacNab classification [21,22], and the presence of back pain, leg pain, and hip pain were determined on postoperative day 10. Patients were also evaluated for the presence of wound infection. Patients who experienced redness, increased temperature, and pain or discharge at the incision line, and those whose infection was detected in microbiological examination and had initiation of antimicrobial treatment were considered patients with wound site infection. ODI scores were re-calculated on postoperative day 30.
OUTCOMES:
The aim of this study was to compare ULBD and BLBD in terms of preoperative (baseline) and postoperative instrumentations, and changes in some of them. Additionally, the improvement success of both surgical procedures in these instruments was investigated separately.
STATISTICS:
The statistical significance level was set at
Between-group analysis of age was performed with the independent sample
Results
DEMOGRAPHIC CHARACTERISTICS:
The study included 142 patients, with 94 undergoing ULBD and 58 undergoing BLBD. Table 1 presents all demographic, clinical, and perioperative characteristics of the patients. In the ULBD group, the mean age was 67.68±9.93 years, with 65.96% (n=62) being female. The BLBD group had a mean age of 66.09±12.32 years, with 60.34% (n=35) being female. No significant differences were observed between the groups regarding age (P=0.382) and sex distribution (P=0.599).
CLINICAL CHARACTERISTICS:
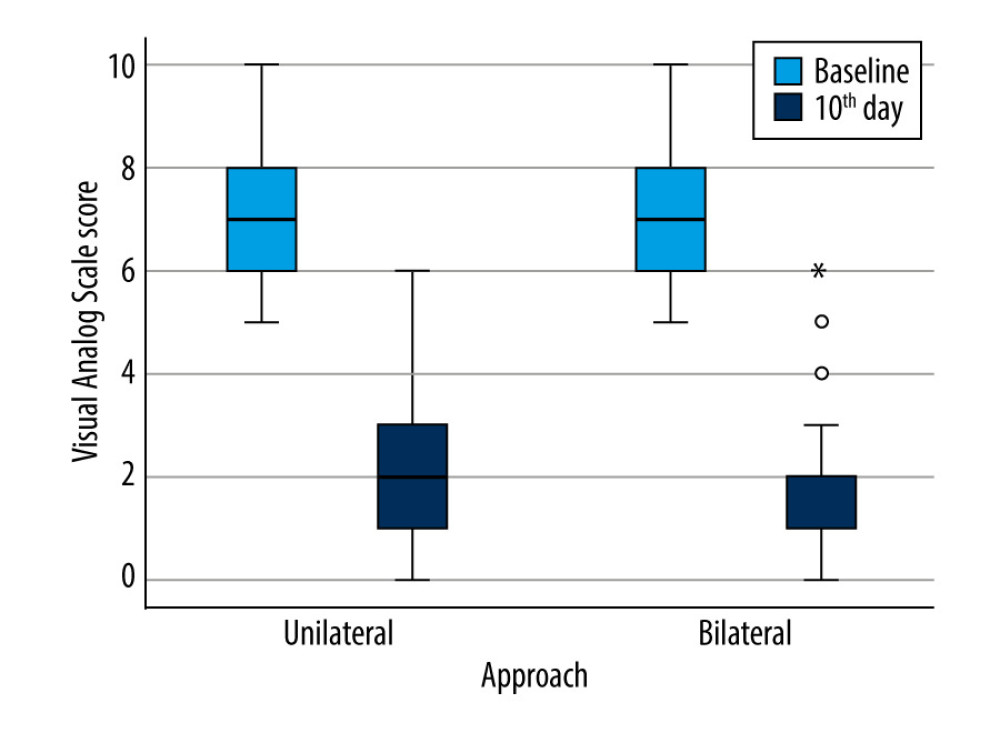
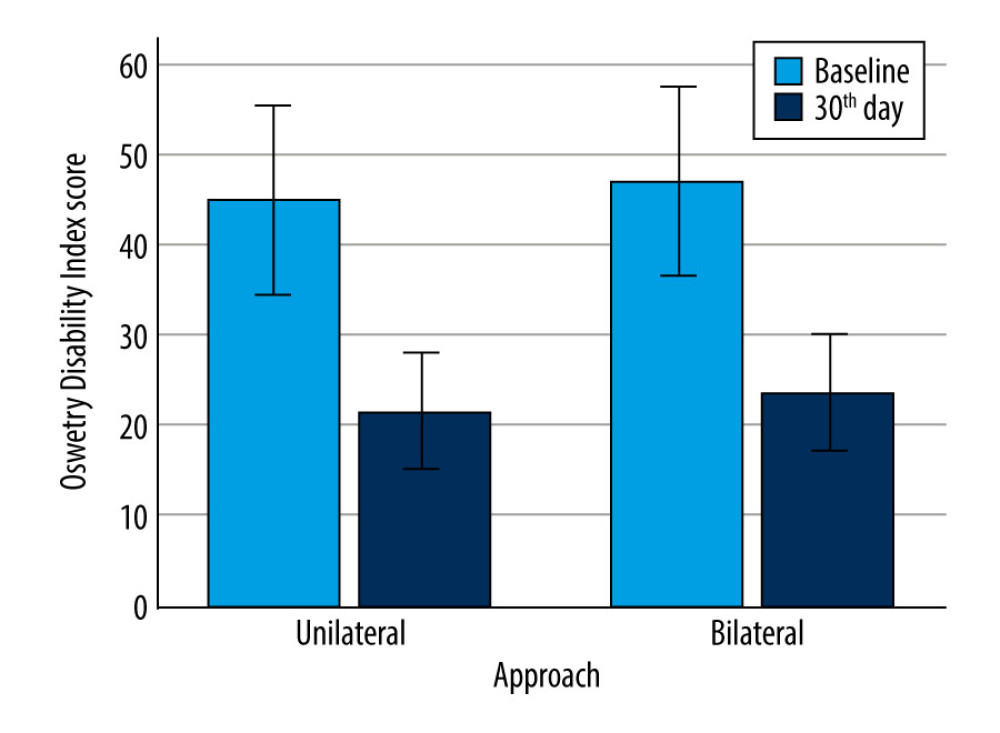
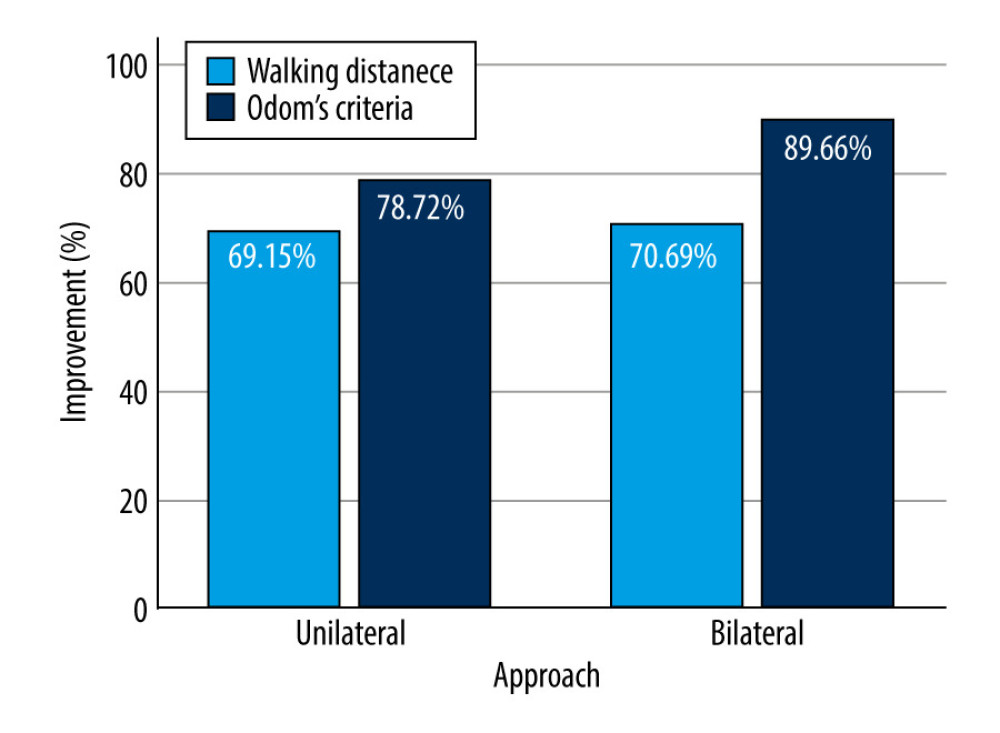
Both groups exhibited a noteworthy reduction in low back pain VAS scores (Figure 1), a significant increase in walking distance, and substantial enhancement in Odom category (Figure 2) on day 10, compared with baseline (P<0.001 for all). Moreover, both groups demonstrated a significant decrease in ODI scores on day 30, compared with baseline (P<0.001 for both). The unilateral approach group exhibited a significantly higher percentage of patients with wound infection (P=0.014), while no wound infections were reported in the bilateral approach group. Although no significant difference was found in the baseline ODI scores between the groups, the ODI score of the unilateral group was significantly lower on day 30 (P=0.047; Figure 3).
Discussion
Surgical intervention becomes imperative when LSS remains unresponsive to conservative treatment. The primary aim of surgery for LSS is to restore the width of the spinal canal [3]. However, aggressive decompression, which can occur with some conventional methods, may lead to iatrogenic spinal instability and other complications [1]. Fusion procedures also have long-term risks, such as pseudoarthrosis and adjacent segment disease [23,24]. Unilateral and bilateral laminotomies for bilateral decompression have been documented to create good outcomes [16,25–28]. This study focuses on the early postoperative outcomes of microscopic ULBD and BLBD, offering a comparative analysis. Both ULBD and BLBD demonstrated notable enhancements in back pain VAS scores, walking distance, and Odom criteria on postoperative day 10, along with improvements in ODI scores on day 30. However, the reduction in ODI score observed with ULBD on day 30 was significantly greater than that of BLBD. Notably, ULBD resulted in a significantly higher incidence of wound site infections than did BLBD.
Hong et al compared unilateral and bilateral laminotomies for decompression of L4–L5 LSS. They found that both techniques provided sufficient decompression of the LSS and significantly reduced pain. However, unilateral laminotomy exhibited advantages, with shorter operating times and reduced blood loss. Additionally, ULBD resulted in less increased translational motion radiologically, suggesting a lower risk of late instability than bilateral laminotomy [29]. In another similar retrospective study, the bilateral and unilateral interlaminar techniques for bilateral decompression among patients with single-level degenerative LSS were compared. They showed that there were no differences in postoperative functional disability and pain between surgical techniques, that significant differences in patient satisfaction and reduction in leg symptoms were unrelated to surgical technique, and that both techniques were safe and effective options for the treatment of patients with single-level degenerative LSS [30]. In a prospective study, the perioperative outcomes of bilateral laminotomy, unilateral laminotomy, and laminectomy were compared. Adequate decompression was achieved in all patients, but the overall complication rate and residual pain were lowest in those who underwent bilateral laminotomy, followed by unilateral laminotomy. Bilateral laminotomy recipients exhibited the highest improvement in walking distance and patient satisfaction, followed by the unilateral laminotomy group. The study reported that unilateral laminotomy provided successful symptomatic relief in 87% of patients at the 9-month follow-up, 82% at the 1-year follow-up, 70% to 88% at the 18-month follow-up, 67% at the 2-year follow-up, and 68% at the 4-year follow-up [8]. In the study by Yaman et al, it was concluded that in both unilateral and bilateral approaches, there was a decrease in postoperative waist and leg pain VAS scores, compared with the preoperative period, bleeding in the bilateral approach, and longer surgery time in the unilateral approach [4]. The use of microscopic imaging made ULBD and BLBD easily performable. Despite their ease of application, differences in practice and potential complications exist between the 2 approaches. BLBD necessitates paraspinal muscle retraction and partial facet joint destruction on both sides, potentially leading to iatrogenic muscle atrophy and denervation abnormalities, contributing to poorer outcomes in spinal stenosis decompression surgery [31–33]. In contrast, ULBD may minimize these complications by causing less damage to the spine’s support structures and preserving the facet joint on the contralateral side. In the present study, both methods provided significant symptomatic and disability improvement in a short time. Although wound infection was more common in ULBD, improvement in disability was more pronounced.
Various studies have compared ULBD and BLBD with traditional laminectomy. Kayalar et al compared ULBD, ULBD and fusion with unilateral instrumentation, and total laminectomy and fusion with bilateral instrumentation. Although no significant differences were found in VAS scores among the groups, ULBD showed advantages in surgery duration, blood loss, and time required for return to work [1]. The study of Liu et al study demonstrated lower rates of atrophy in multifidus cross-sectional areas and postoperative back pain VAS scores in the ULBD group than did conventional laminectomy at a 2-year follow-up [34]. Another study indicated that bilateral spinal canal decompression with a unilateral approach reduced surgical trauma, blood loss, complication rates, and hospital stay, compared with the bilateral approach [35]. The 5-year patient-reported outcomes for wide laminectomy, segmental bilateral laminotomy, or unilateral hemi-laminectomy were presented in a cohort study. The results showed no significant differences in patient-reported outcome measures, reoperation rates, or time to reoperation between the surgeries [25]. A recent review by Moughal et al underscored ULBD’s preservation of the osteoligamentous complex, suggesting shorter operating times, less blood loss, and comparable clinical outcomes to classical laminectomy. However, the review highlights challenges in drawing universally acceptable conclusions due to the retrospective nature or lack of comparison groups in most studies [26]. Ulrich et al compared ULBD with the standard open midline approach for bilateral decompression, concluding that both approaches offered effective treatment results at the 3-year follow-up. Nevertheless, ULBD presented technical challenges in terms of changes in spinal stenosis symptoms and function [16]. In a prospective, randomized trial comparing ULBD with open laminectomy for degenerative LSS, short-term follow-up demonstrated that microscopic ULBD was as effective as open decompression. ULBD provided additional benefits, including a significantly greater reduction in pain VAS score, postoperative recovery time, mobilization time, and recovery time, compared with open surgery [27]. Cheb et al compared full endoscopic laminotomy and ULBD for bilateral decompression of the L4–L5 LSS. They demonstrated that the endoscopic approach was comparable to ULBD in terms of clinical and radiological outcomes, with improved recovery for single-level LSS, and could further reduce tissue damage and accelerate postoperative recovery [36]. ULBD may have the advantage of shorter operative time compared to conventional laminectomy in terms of decompression in single-level degenerative LSS, but this advantage does not appear to translate to superiority in terms of back pain, functional outcome, and quality of life [28]. Nonetheless, ULBD has been reported to have better results in terms of postoperative back pain, but in this study the operation time was longer [37], which may suggest that surgeon experience and approach can play a large role in outcomes, as demonstrated previously in studies examining different approaches to surgical treatment [38,39].
Classical laminectomy poses risks, including damage to supraspinous and interspinous ligaments, leading to iatrogenic spinal instability and partial removal of facet joints, resulting in spondylolisthesis [40,41]. ULBD, with its more limited damage to these structures, presents a lower risk of iatrogenic instability. Reported advantages of ULBD include shorter operating time, shorter postoperative hospital stay, earlier ambulation, lower risk of adjacent segment degeneration, and lower risk of muscle atrophy due to unilateral opening of paravertebral muscles compared to bilateral opening, causing less blood loss and reducing the time to initiate mobilization. Additionally, the ULBD approach has been reported to provide better visualization of the contralateral recess and to allow for bilateral discectomy if necessary [17,31,35,42,43]. While our study did not compare classical laminectomy and microscopic laminotomy, the collective results from our study and previous research suggest that ULBD and BLBD can achieve satisfactory success in patients with LSS requiring bilateral decompression, without exposing patients to the potential high complication risks of laminectomy. ULBD may be more successful than BLBD in improving disability. However, some researchers assert that ULBD is technically more challenging, has a longer learning curve, presents a higher risk of dural sac lesions and liqueuric fistula due to instrument manipulation through a small portal, has a poorer view of the contralateral recess, and has higher rates of recurrence and reoperation due to inadequate decompression, compared with open surgery or the bilateral approach [15–17]. Our study also indicated that ULBD can pose a higher risk for wound infection than BLBD. This disadvantage could potentially be mitigated as surgeons gain more experience with ULBD, leading to fewer traumatic manipulations and shorter operating times. Comprehensive longitudinal studies are necessary to establish generally accepted conclusions regarding the advantages and disadvantages of ULBD over BLBD and classical laminectomy, enabling patients with LSS to improve their symptoms and quality of life with a less traumatic procedure.
The study has inherent limitations typically associated with retrospective studies. Being a single-center study with a relatively small number of participants, conclusions regarding the efficacy of these approaches are not generalizable. It is possible that the use of different approaches to the surgeries and different experience levels among surgeons could alter the outcomes of the interventions. Additionally, some parameters investigated in previous studies comparing LSS procedures, such as LSS pathological types, radiological degree of canal stenosis, surgery times, bleeding amounts, complications, long follow-up periods, ambulation time, and surgeon experience, were not examined. However, the primary objective of the study was to assess the 2 methods and provide evidence regarding their outcomes among patients with single-level LSS who did not benefit from conservative treatment. Therefore, the present data are valuable to report as a single-center experience.
Conclusions
To summarize, we demonstrated that both the ULBD and BLBD procedures demonstrated significant improvement in pain and disability among patients with single-level LSS at short-term follow-up. While there was no significant difference in pain reduction success between the 2 procedures, ULBD provided significantly greater improvement in disability. However, the risk of developing wound infection was greater among ULBD recipients. ULBD appears to be a less invasive, more successful, and potentially safer surgical alternative to BLBD and classical laminectomy for patients with single-level LSS, provided extra precautions are taken regarding wound infection.
References
1. Kayalar AE, Mammadkhanli O, Canbay S, Naderi S, Comparison of three different surgical treatment procedures used in the treatment of lumbar spinal stenosis; retrospective clinical study: J Turk Spinal Surg, 2020; 31(1); 11-17
2. Katz JN, Zimmerman ZE, Mass H, Makhni MC, Diagnosis and management of lumbar spinal stenosis: A review: JAMA, 2022; 327(17); 1688-99
3. Iacob G, Salam A, Hawis AR, Techniques of surgery for lumbar spinal stenosis: A comparative study: Romanian Neurosurgery, 2018; XXXII; 240-61 Available from: http://journals.lapub.co.uk/index.php/roneurosurgery/article/view/1089/968
4. Yaman O, Ozdemir N, Dagli AT, A comparison of bilateral decompression via unilateral approach and classic laminectomy in patients with lumbar spinal stenosis: A retrospective clinical study: Turk Neurosurg, 2015; 25(2); 239-45
5. Debbag S, Yalcinkaya A, Saricaoglu F, Nociceptive improvements and kynurenine pathway alterations with diclofenac treatment in a rat model of neuropathic pain created by partial sciatic nerve ligation: Eur Rev Med Pharmacol Sci, 2023; 27(9); 4239-47
6. Ohtomo N, Nakamoto H, Miyahara J, Comparison between microendoscopic laminectomy and open posterior decompression surgery for single-level lumbar spinal stenosis: A multicenter retrospective cohort study: BMC Musculoskelet Disord, 2021; 22(1); 1053
7. Machado GC, Ferreira PH, Yoo RI, Surgical options for lumbar spinal stenosis: Cochrane Database Syst Rev, 1996; 2016(11); CD012421
8. Thomé C, Zevgaridis D, Leheta O, Outcome after less-invasive decompression of lumbar spinal stenosis: A randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy: J Neurosurg Spine, 2005; 3(2); 129-41
9. Young S, Veerapen R, O’laoire SA, Relief of lumbar canal stenosis using multilevel subarticular fenestrations as an alternative to wide laminectomy: Preliminary report: Neurosurgery, 1988; 23(5); 628-33
10. McCulloch JA: Microsurgical spinal laminotomies in the adult spine, 1991, New York (NY), Principles and Practice
11. Moughal S, Quaye MC, Wahab S, Unilateral microscopic approach for lumbar spinal stenosis decompression: A scoping review: Eur Spine J, 2023; 32(2); 475-87
12. Cavuşoğlu H, Türkmenoğlu O, Kaya RA, Efficacy of unilateral laminectomy for bilateral decompression in lumbar spinal stenosis: Turk Neurosurg, 2007; 17(2); 100-8
13. Choi WS, Oh CH, Ji GY, Spinal canal morphology and clinical outcomes of microsurgical bilateral decompression via a unilateral approach for lumbar spinal canal stenosis: Eur Spine J, 2014; 23(5); 991-98
14. Takahashi H, Aoki Y, Saito J, Unilateral laminectomy for bilateral decompression improves low back pain while standing equally on both sides in patients with lumbar canal stenosis: Analysis using a detailed visual analogue scale: BMC Musculoskelet Disord, 2019; 20(1); 100
15. Ang CL, Phak-Boon Tow B, Fook S, Minimally invasive compared with open lumbar laminotomy: No functional benefits at 6 or 24 months after surgery: Spine J, 2015; 15(8); 1705-12
16. Ulrich NH, Burgstaller JM, Gravestock I, Outcome of unilateral versus standard open midline approach for bilateral decompression in lumbar spinal stenosis: Is “over the top” really better? A Swiss prospective multicenter cohort study: J Neurosurg Spine, 2019 [Online ahead of print]
17. Soares GG, Unilateral laminotomy for bilateral microdecompression of stenosis of the lumbar canal: Coluna/Columna, 2015; 14(3); 236-39
18. Odom GL, Finney W, Woodhall B, Cervical disk lesions: J Am Med Assoc, 1958; 166(1); 23-28
19. Fairbank JC, Pynsent PB, The Oswestry disability index: Spine (Phila Pa 1976), 2000; 25(22); 2940-53
20. Assaker R, Lumbar laminectomy: Classical versus minimally invasive surgical technique: Surgery of the Spine and Spinal Cord: A Neurosurgical Approach, 2016; 497-512 Approach. 2016;497-512. Available from:https://link.springer.com/chapter/10.1007/978-3-319-27613-7_32
21. Macnab I, Negative disc exploration: An analysis of the causes of nerve-root involvement in sixty-eight patients: JBJS, 1971; 53(5); 891-903
22. Turner JA, Ersek M, Herron L, Deyo R, Surgery for lumbar spinal stenosis: Attempted meta-analysis of the literature: Spine, 1992; 17(1); 1-8
23. Muggleton JM, Kondracki M, Allen R, Spinal fusion for lumbar instability: Does it have a scientific basis?: J Spinal Disord, 2000; 13(3); 200-4
24. Kanayama M, Hashimoto T, Shigenobu K, Intraoperative biomechanical assessment of lumbar spinal instability: Validation of radiographic parameters indicating anterior column support in lumbar spinal fusion: Spine (Phila Pa 1976), 2003; 28(20); 2368-72
25. Bouknaitir JB, Carreon LY, Brorson S, Wide laminectomy, segmental bilateral laminotomies, or unilateral hemi-laminectomy for lumbar spinal stenosis: five-year patient-reported outcomes in propensity-matched cohorts: Spine (Phila Pa 1976), 2021; 46(21); 1509-15
26. Moughal S, Quaye MC, Wahab S, Unilateral microscopic approach for lumbar spinal stenosis decompression: A scoping review: Eur Spine J, 2023; 32(2); 475-87
27. Mobbs RJ, Li J, Sivabalan P, Outcomes after decompressive laminectomy for lumbar spinal stenosis: Comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article: J Neurosurg Spine, 2014; 21(2); 179-86
28. Ko S, Oh T, Comparison of bilateral decompression via unilateral laminotomy and conventional laminectomy for single-level degenerative lumbar spinal stenosis regarding low back pain, functional outcome, and quality of life – a randomized controlled, prospective trial: J Orthop Surg Res, 2019; 14(1); 252
29. Hong SW, Choi KY, Ahn Y, A comparison of unilateral and bilateral laminotomies for decompression of L4–L5 spinal stenosis: Spine (Phila Pa 1976), 2011; 36(3); E172-78
30. Den Boogert HF, Keers JC, Marinus Oterdoom DL, Kuijlen JM, Bilateral versus unilateral interlaminar approach for bilateral decompression in patients with single-level degenerative lumbar spinal stenosis: A multicenter retrospective study of 175 patients on postoperative pain, functional disability, and patient satisfaction: J Neurosurg Spine, 2015; 23(3); 326-35
31. Mayer TG, Vanharanta H, Gatchel RJ, Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients: Spine (Phila Pa 1976), 1989; 14(1); 33-36
32. See D, Kraft G, Electromyography in paraspinal muscles following surgery for root compression: Arch Phys Med Rehabil, 1975; 56(2); 80-83
33. Sihvonen T, Herno A, Paljärvi L, Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome: Spine, 1993; 18(5); 575-81
34. Liu X, Yuan S, Tian Y, Modified unilateral laminotomy for bilateral decompression for lumbar spinal stenosis: Technical note: Spine (Phila Pa 1976), 2013; 38(12); E732-37
35. Krut’ko AVResults of decompressive-stabilizing procedures via unilateral approach in lumbar spinal stenosis: Zh Vopr Neirokhir Im N N Burdenko, 2012; 76(2); 33-40 [in Russian]
36. Chen K-T, Choi K-C, Shim H-K, Full-endoscopic versus microscopic unilateral laminotomy for bilateral decompression of lumbar spinal stenosis at L4–L5: Comparative study: Int Orthop, 2022; 46(12); 2887-95
37. Gomaa AF, A comparative study between traditional full laminectomies and microsurgical bilateral decompression by unilateral approach ın treatment of lumbar canal stenosis. J: Cardiovasc Dis Res, 2021; 12(3); 2851-59
38. Yalcinkaya A, Yalcinkaya A, Atici SDT E H Study Collaboration, Local excision versus thrombectomy in thrombosed external hemorrhoids: A multicenter, prospective, observational study: BMC Surg, 2023; 23(1); 228 Erratum in: BMC Surg. 2023;23(1):321
39. Kelz RR, Sellers MM, Niknam BA, A National comparison of operative outcomes of new and experienced surgeons: Ann Surg, 2021; 273(2); 280-88
40. Phan K, Mobbs RJ, Minimally ınvasive versus open laminectomy for lumbar stenosis: A systematic review and meta-analysis: Spine (Phila Pa 1976), 2016; 41(2); E91-E100
41. Tuite GF, Stern JD, Doran SE, Outcome after laminectomy for lumbar spinal stenosis. Part I: Clinical correlations: J Neurosurg, 1994; 81(5); 699-706
42. Banczerowski P, Czigléczki G, Papp Z, Minimally invasive spine surgery: Systematic review: Neurosurg Rev, 2015; 38; 11-26
43. Moisi M, Fisahn C, Tkachenko L, Unilateral laminotomy with bilateral spinal canal decompression for lumbar stenosis: A technical note: Cureus, 2016; 8(5); e623
Figures
In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952